Estimation of hemoglobin purpose of the test and their method
Hemoglobin (Hb) is the main component of red blood cells and is a conjugated
protein. A molecule of Hb contains two pairs of polypeptide chains α2 β2 and
four haem groups each having an atom of ferrous iron. The oxygen-carrying
capacity of Hb when fully saturated is 1.34 ml/g. Approximately 34% of the RBCs
by weight is Hb. Iron content of Hb is 0.347 gm/100 g. The main function of Hb
is to transport oxygen from the lungs to the tissues.
There are various forms of Hb as under :
There are various forms of Hb as under :
i.
Oxyhemoglobin (Hb O2)
ii.
Carboxy hemoglobin (Hb CO)
iii.
Sulfhemoglobin (SHb)
iv.
Methemoglobin (Hi)
Measurement of the concentration of Hb in the
blood is known as hemoglobinometry.
Types of blood samples used for Hb
estimation are
i. Capillary blood from a finger prick.
ii. Intravenous
sample—It should be well anticoagulated, preferably in EDTA. Liquid
anticoagulants should not be used at all as these dilute and decrease Hb
concentration.
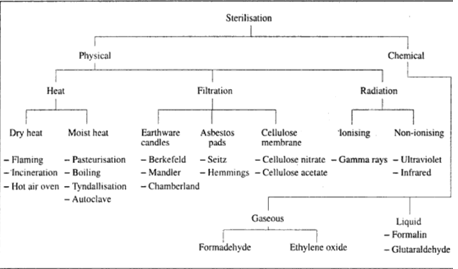
METHODS FOR ESTIMATION OF HAEMOGLOBIN Various
methods used for estimation of Hb are divided into 4 groups as under
I.
Colorimetric method: Colorimetric method is based on colorimetric measurement of
the intensity of color developed on addition of some substance to the blood.
Colorimetric methods include the following:
1. Cyanmethaemoglobin method
2.
Oxyhaemoglobin method
3. Electronic counter method
4. Direct reading electronic
haemoglobinometer
5. Sahli’s method
II. Measurement of O2 carrying capacity of
Hb: Measurement of O2 carrying capacity of Hb can not be used for mass
screening but is used in referral or research laboratories only.
III.
Measurement of iron content of Hb: Measurement of iron content of Hb is used
only for research purposes.
IV. Specific gravity method: It is a very rapid
method and is useful for screening blood donors for anemia in the blood donation program. The normal specific gravity of blood ranges from 1.048-1.066. Some of
the commonly used methods are discussed below.
ESTIMATION OF HEMOGLOBIN
The purpose of estimating hemoglobin is to determine the oxygen-carrying capacity of the blood. The results help in detecting diseases that cause deficiency or excess of hemoglobin. Hemoglobin estimation also helps to incite changes in the hemoglobin concentration before and after operation and blood transfusion.- Several techniques have been used to determine hemoglobin in the form of oxyhemoglobin, carboxyhemoglobin, cyanmethaemoglobin, acid and alkaline haematin, based on their oxygen-carrying capacity, iron content or color.
- Hemoglobin is expressed as grams per liter, grams per 100 ml or grams per decilitre (dl) of blood. A major problem inaccurate measurement of hemoglobin content is the nonavailability of a suitable standard.
- Some visual methods, such as Sahli's, use an artificial standard. However, in 1966, the International Committee for Standardisation in Hematology (ICSH) recommended cyanmethaemoglobin, prepared according to strict specifications, as a suitable standard.
- Cyanmethaemoglobin is very stable and the standard is available commercially
Estimation of hemoglobin by Acid Haematin Method (Sahli method)
1. Acid Haematin Method (Sahli)
-This is a visual method of hemoglobin estimation, and is not very accurate. Visual methods are now used only in the areas of the world where electricity is not available.Principle of Acid Haematin Method (Sahli)
Hemoglobin is converted into acid haematin by the action of hydrochloric acid. The brown color of the compound is matched visually against a brown glass standard in a comparator. |
Acid Haematin Method (Sahli) |
Specimen
The sample maybe venous blood collected in EDTA or oxalate anticoagulant; or blood obtained by capillary puncture.Apparatus and reagent
1. Sahli graduated tube and haemoglobinometer percentage (14.6 g =
100 %).
2.0.1 N Hydrochloric acid.
3. Hemoglobin pipette marked at 20 cu.mm (ul) or 0.02 ml.
hemoglobinometer consisting of the comparator with glass standards. One side of the tube gives the reading in grams of Hb/100 ml blood while the other side gives it as a percentage (14.6 g = 100 %).
 |
Acid Haematin Method (Sahli) |
Technique:
Fill the graduated tube up to mark 20 with 0.1 N HCI.
- Fill hemoglobin pipette exactly up to the 20 cu.mm, mark with well-mixed blood by gentle controlled sucking, holding the pipette horizontal.
- Wipe off the blood on the outside of the pipette with a piece of gauze.
- Empty the pipette into the acid in the tube gently without causing bubbles.
- Rinse the pipette 2-3 times by drawing in and discharging the fluid. Mix the acid haematin solution in the tube and allow to stand for 5-10 minutes.
- Place the tube in the Sahli comparator and start adding 0.1 N HCl or distilled water drop by drop.
- Mix between each addition, continue till the color matches that of the standard. Read the volume of solution in the graduated tube, and express as grams/100 ml (g/dl) or as a percentage.
Note:- Care should be taken to clean the hemoglobin pipette with distilled water by sucking in and discharging water several times. It should be dried with acetone or alcohol before reuse.
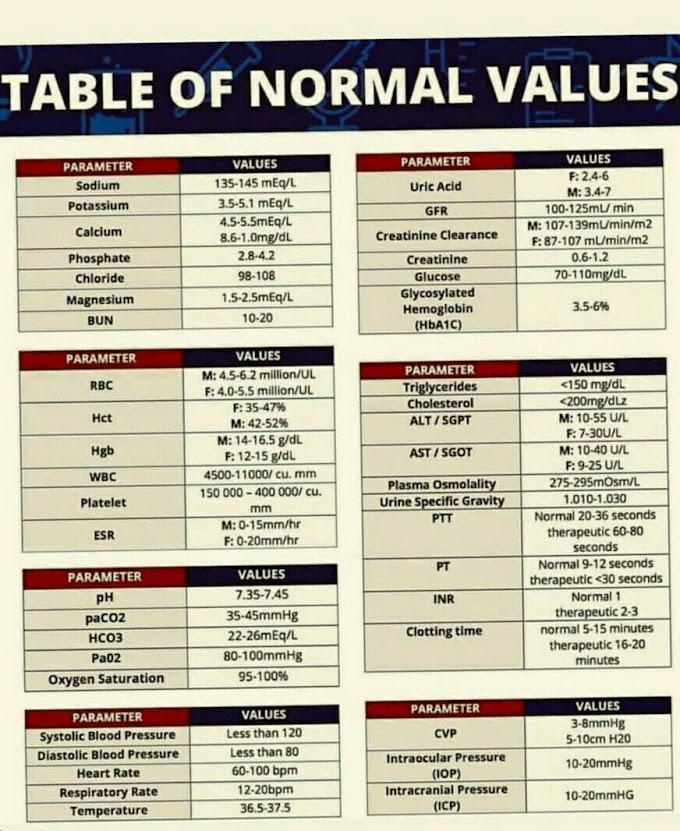
Normal Values of Hemoglobin
Men 15 ± 2 g/dlWomen 13.5 ± 1.5 g/dl
Infants 16.5 ± 3 g/dl
Advantages
|
Disadvantages
|
i. Simple bedside test.
|
i. There can be visual errors.
|
ii. Reagents and apparatus are cheap.
|
ii. Carboxy met and sulfhaemoglobins cannot be converted
to acid haematin.
|
iii. The comparator can fade over the years.
|
|
iv. Color of acid haematin also fades quickly.
|
|
Other methods like carboxy Hb and alkali haematin
methods are not used these days.
|
|
Errors in Haemoglobinometry
Errors in Haemoglobinometry
|
|||
1. Sampling error:
|
2. Error in method:
|
3. Error in equipment:
|
|
| Improper venipuncture technique e.g. More squeezing can alter the results, or the reading may be affected by the type of anticoagulant used. |
Results are better with cyanate and oxy Hb method. In Sahli’s method, the
chances of error are more. |
These could be due to the quality of the material of the equipment or calibration of the equipment. | This could be because of improper training, lack of familiarity |
Estimation of hemoglobin by Cyanmethaemoglobin Method
-
This is a colorimetric method, and therefore, more accurate than Sahli's. A
commercial cyanmethaemoglobin standard is used for comparison. |
| Estimation of hemoglobin by Cyanmethaemoglobin Method |
Principle:-
- The hemoglobin is treated with a reagent containing potassium ferricyanide, potassium cyanide, and potassium dihydrogen phosphate.
- The ferricyanide forms methemoglobin which is converted to cyanmethaemoglobin by cyanide.
- All forms of hemoglobin except sulfhaemoglobin is converted to cyanmethaemoglobin. Reagents
1.Drabkin's solution
- Potassium cyanide 500 mg
- Potassium ferricyanide 200 mg
- Potassium dihydrogen phosphate 140 mg
- Distilled water 1 liter
- PH -7.0-7.4
Store in a dark bottle. The solution keeps for several
months.
 |
| Estimation of hemoglobin by Cyanmethaemoglobin Method |
Cyanmethaemoglobin standard:
- It is available commercially in sealed ampoules. The concentration is indicated on the label and is usually about 60 mg per 100 ml.
 Technique:
Technique:
- Add 0.02 ml (20
ul) of blood to 5 ml of Drabkin's solution in a test tube (1:250 dilution).- Mix well and allow standing for 10 minutes. Read the absorbance colorimetrically at 540 nanometers
- (green filter) with Drabkin's solution as blank. Read the absorbance of the standard in the same way.
- Alternatively, a calibration curve may be prepared by diluting the standard 1:2, 1:3 and 1:4; and the concentration plotted against the absorbance.
The concentration of the hemoglobin in the blood can then be measured from its absorbance.
Advantages
|
Disadvantages
|
i.
The method is simple and quick.
|
i. It does not measure sulfhaemoglobin.
|
ii. The result is not affected by the rise of plasma bilirubin.
|
ii. The standard is not stable.
|
iii.
Most forms of hemoglobin’s
(i.e. HBO, Hi, and HbCO) are measured in this method.
|
iii. Increased absorbance may be caused by
turbidity due to hyperlipidaemia, leucocytosis (>30x109/L) and abnormal
plasma proteins.
|
Cyanmet Hb Method
This is the best method for Hb estimation and it has been recommended by the International Committee for Standardization in Haematology (ICSH).Principle
- Blood is diluted in a solution called Drabkin’s fluid containing potassium ferricyanide and potassium cyanide (KCN).
- The oxy, carboxy and met Hb are all converted into cyanmet Hb (HiCN) and there is development of pink color.
- The intensity of pink color can be measured in a spectrophotometer or photoelectric colorimeter at 540 nm and this is compared with that of a standard cyanmethaemoglobin solution.
Reagents
Drabkin’s fluid can be prepared as under:Potassium ferricyanide : 0.2 g
Potassium cyanide : 0.05 g
Dihydrogen potassium phosphate : 0.14 g
Distilled water : 1000 ml
Drabkin’s fluid should be clear and pale yellow having a pH of 7.0-7.4.
Procedure „
- Add 20 μl (0.02 ml) of blood to 5 ml of Drabkin’s solution in a test tube (1:251 dilution). „ Mix well and allow it to stand for 3-5 minutes. „
- Take a reading of the test and standard in a spectrophotometer or photoelectric colorimeter at 540 n.
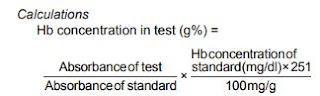
Calculations Hb concentration in test (g%)
Advantages :
i. There is no chance of visual error.ii. All forms of Hb except sulfhaemoglobin can be measured.
iii. The standard is very stable.
Disadvantages:
i. We cannot take the reading immediately.ii. If blood is turbid due to plasma proteins, hyperlipidemia, leukemias, the absorbance is more and hence incorrect results may be obtained.
iii. Results are affected due to hyperbilirubinemia.
Oxyhaemoglobin Method
This is a simple and quick method and results are not affected by hyperbilirubinemia. Principle Blood is diluted in a solution of ammonia. There is the development of reddish pink-color which is measured in a spectrophotometer or photoelectric colorimeter at 625 nm and compared with that of a standard oxyHb solution.Procedure „
- Add 20 μl (0.02 ml) of blood to 4 ml of 0.4 ml/l ammonia solution in a test tube. „
- Use a tight-fitting stopper and mix by inverting the tube several times. „
- Take reading of test and standard in a spectrophotometer or photoelectric colorimeter with a yellow or green filter (625 nm).
Calculations As for cyanmet method.
Advantages:
i. The method is simple and quick.ii. The result is not affected by rise of plasma bilirubin.
iii. Most forms of hemoglobins (i.e. HbO, Hi, and HbCO) are measured in this method.
Disadvantages:
i. It does not measure sulfhaemoglobin.ii. The standard is not stable.
iii. Increased absorbance may be caused by turbidity due to hyperlipidemia, leucocytosis (> 30x109/L) and abnormal plasma proteins.
Electronic Counter Method
This is a multi-parameter determining electronic equipment.Principle
The method is based on electrical impedance principle. The blood is diluted with isoton and lysate which lyses the RBCs converting Hb into cyanmethaemoglobin and its concentration is measured in the spectrophotometer at 540 nm. In some instruments, the cyanmethaemoglobin method is replaced with another method employing a non-toxic chemical, sodium lauryl sulfate.Disadvantage :
i. High white cell count (> 30,000/μl) produces false elevation of Hb.Direct Reading Electronic Haemoglobinometers
These have inbuilt filters. Reading of Hb in g/dl is visualized on the screen which may have light-emitting diode (LED) display or analog meter. These equipment work on the principle of cyanmetHb, oxyHb method or color comparators in which color of blood is compared Photoelectric colorimeter used for taking reading of hemoglobin in cyanmet Hb method and oxyhemoglobin method.without conversion to a derivative, against a range of colors which represent hemoglobin concentration.
Disadvantage
i. Calibration of the instrument can be faultyClinical significance
A low hemoglobin level indicates anemia. Estimates of Hgb in
each RBC are moderately important when determining the total blood Hgb.
However, hemoglobin findings are even more dependent upon the total number of
RBC's. In other words, for the diagnosis of anemia, the number of RBC's is as
important as the hemoglobin level.
A lack of available iron causes one type of anemia, due to
the reduced production of hemoglobin. Remember that in the strictest sense,
anemia is not in itself a diagnosis, but rather a symptom that there is
something else wrong in the body. For example, malnutrition (low iron levels),
would be the diagnosis of the patient, not just the anemia. The secondary
diagnosis would be anemia, but malnutrition must be treated in order to
"cure" the anemia.
Clinical significance |
|
Low Hemoglobin value indicate
|
high Hemoglobin value indicates
|
|
|
QUALITY CONTROL IN HAEMOGLOBIN ESTIMATION
- For reliability of the results, quality assurance or quality control is a must. It includes proficiency in the collection, labeling, storage and results of the test.
- Quality control has three components: internal quality control, standardization and external quality control.
- Precision refers to reproducibility of a result but a test may be precise without being accurate. Inaccuracy occurs as a result of the improper standards, reagents, calibration of equipment and poor technique.
- Accuracy is attained by the use of reference material which has been assayed by different methods and in different laboratories.








If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..