Quality Assurance System, External and Internal Quality assurance
Quality Assurance System
They are:
2. Analytical factors:
3. Post analytical factors:
PRE ANALYTICAL FACTORS
1. Patient Identification and Preparation
2. Specimen Collection, Transportation and Storage
3. Specimen Receiving and Recording in the Laboratory
ANALYTICAL FACTORS
- Internal Quality ControlMaintenance of equipmentReagents, standards and calibratorsControl materialLinear rangeMethod evaluationMeasurement of inaccuracyApplication of quality control systemControl rulesExternal Quality Control
POSTANALYTICAL FACTORS
Quality Assurance System
Quality
assurance system (QAS) can be defined as all the systematic actions necessary
to provide adequate confidence that laboratory services will satisfy given
medical needs for patient care. It encompasses factors in three different
areas.
They are:
1.
Preanalytical factors: These factors occur outside the laboratory and include
patient preparation and collection, handling and storage of specimens before
processing.
2. Analytical factors: These can be controlle by an efficient quality control system within the laboratory by recognising and minimising analytical errors.
3. Postanalytical factors: These consist of recording and transmitting patient data to the physician in a fashion which can be interpreted correctly.
- Therefore, delivery of accurate results is an outcome of co-ordinated interdepartmental group approach. Besides accuracy in laboratory testing, other quality characteristics involve non-laboratory personnel such as physicians, nursing staff and clerical staff.
- Those outside the laboratory help in the QAS by providing effective test request forms, clear instructions for patient preparation and specimen handling and appropriate time interval for specimen processing, testing and result reporting so that result reports can be sent to the physician with reference ranges for proper interpretation and patient care.
PREANALYTICAL FACTORS
1. Patient Identification and Preparation
Before a
sample is taken, the patient should be positively identified by verifying his
name and identification number.
- The laboratory should provide a procedure manual containing information regarding each test, from how to request a test to any instructions that should be followed before and while a sample is being collected.
- This manual should be available to all medical and nursing staff. Patient preparation may include instructions about nutritional status, alcohol, drugs, smoking, exercise and sleep.
2. Specimen Collection, Transportation and Storage
The method
and time of specimen collection depend on the nature of the test requested. The
laboratory guidelines in the manual should be strictly adhered to for specimen
collection.
- The type of anticoagulant used for blood samples and containers used will vary with the nature of the test. It may be necessary to use more than one sample containers per patient. Each tube should be labelled with patient's name, identification number, and the date and time of sample collection.
- Once collected, the specimens should reach the laboratory in a timely manner without unnecessary delay. Sometimes, the temperature at which the specimen should be transported is also critical.
3. Specimen Receiving and Recording in the Laboratory
When a
sample arrives in the laboratory, it should be received either by logging in
the computer or by recording in a register with a laboratory reference number.
ANALYTICAL FACTORS
After the
samples are properly logged in and distributed for testing, analytical system
checks are implemented to ensure that the results are accurate.
Quality
control should set limits and directions for the laboratory scientists involved
in performance of the test. This can be achieved by constantly monitoring the
quality control system through:
1. Internal quality control.
2. External quality control.
Internal Quality Control
The internal
quality control can be maintained by going through a complete checklist of
items to make sure that all laboratory systems are being monitored and in
control. This checklist includes:
(i)
Maintenance
of equipment and glassware
(ii)
Quality control of reagents, standards,control
materials and reference ranges.
(iii)
Method
selection and evaluation
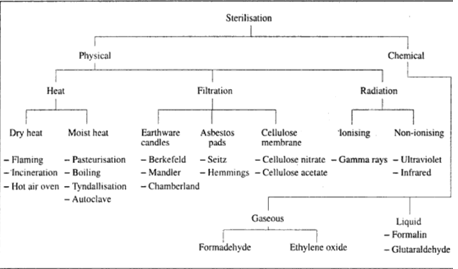
Maintenance of equipment
• To ensue that all instruments are performing up to
expected standards, a schedule of daily and monthly preventive maintenance for
each piece of equipment is essential.
- A scheduled maintenance sheet for each instrument should be available for the regular check-up of operating instructions. Tolerance limits for each test should be specified so that malfunctions can be detected.
- The temperature of all thermostatically controlled instruments such as water baths, refrigerators and freezers, incubators, ovens, autoclaves and dry heating blocks should be recorded daily or just before use.
- Balances, mechanical pipettes and glass pipettes should be properly maintained and calibrated on regular basis. Glassware should be cleaned properly and discarded when it becomes chipped or cracked.
Reagents, standards and calibrators
- Reagents and kits should be dated when prepared orreceived; and also when they are brought in use. New lots of reagents should run in parallel with old reagent lots before being used for analysis.
- The dependability of a method to give reliable results depends on the quality of the reagents used for calibration and standardisation. The most highly purified chemicals should be used.
- For some analyses, certified reference materials (CRM) are used to develop, verify and calibrate the reference methods. The calibrators should have their concentrations assigned through the use of either reference methods or other very specific methods.
The comparative analysis of the calibrator and the specimens provides the basis for calculating values for patientspecimens.
Control material
Control materials should be analysed as unknown samples to monitor calibration of methods and instrumentation. The same tect the specific analyte of interest. Specificity can be expressed as:
where TN is
true negative and FP is false positive.
Linear range Linear range is the concentration
range over which the measured concentration is equal to the actual
concentration without modification of the method. A wide linear range is
preferred.
Method evaluation In method evaluation, imprecision
and inaccuracy of a method are determined and compared with the maximum error
all-owed on the basis of medical criteria. If they fall outside the limit, the
test is either rejected or modified.
Measurement
of imprecision Imprecision is the dispersion of repeated measurements around
the mean and is due to the presence of random analytical error. It is the
inability to produce the same result from the same specimen on repeated
estimations. Imprecision can be detected by analysing a group of patient
specimens along with controls over a period of 20 days. Once the data is
collected, the level of imprecision can be determined
Measurement of inaccuracy Inaccuracy is the difference between
the measured value and its true value and is due to systematic analytical
error. If the degree of imprecision is acceptable, the degree of inaccuracy can
be estimated by comparison-ofmethods experiment. In this method, the same
patient samples are tested by the method being evaluated and by a comparative
method. The best comparative method is the reference method which has
negligible inaccuracy. However, reference methods are very laborious and may
need specialised equipment. Therefore, the results of the new test method are
usually compared with those of the method in routine use. At least 40 to 100
samples must be run by both methods before reaching a conclusion. The results
can be interpreted either by plotting the graph using the data obtained by both
the methods to decide the degree of inaccuracy: or by applying the 'F' and 7'
test (refer to Section I Chapter 4). Figure 5.1 shows the schematic
representation of control data showing no analytical error (A): increased
random error (B) and increased systematic error (C).
Application of quality control system
The purpose of quality control system is to monitor analytical processes, detect analytical errors during analysis and prevent reporting of incorrect patient results. The monitoring is usually done by analysing stable control materials and then comparing the observed values with the expected values. The different levels of control material should be evaluated for at least 20 days. The means (X) and standard deviation (SD) of these control data are then calculated. Control values may be compared with statistical limits numerically or by display on a control chart. This chart is an extension of Gaussian distribution. The vertical axis (y-axis) is labelled with the control values and the horizontal axis (x-axis) is labelled with the days. The y-axis is scaled to provide a concentration range from x3SD to X + 3 SD. Each control result is plotted as a point intersecting the control SD and the day of the test (Fig. 5.2).
An
analytical method is said to be in control when there is a symmetrical
distribution of control values about the mean, and there are few values of
control outside the 2 SD limits. A sudden jump from the established mean to a
new mean is considered a 'shift'; whereas a slow deviation from the mean value
in either direction is considered a "trend'.
Each
laboratory may decide its own criteria for judging whether control results are
acceptable or not.
There are
some popular control rules which can help in decision-making.
Control rules
1. One control observation exceeds mean + 2
SD. This is
a warning rule.
2. One
control observation exceeds the mean
3 SD. This
is a rejection rule.
3. Two
consecutive control observations are on the same side of the mean and exceed
mean + 2 SD control limits. This is a rejection rule.
4. The
difference between two control observations within one run exceeds + 4 SD. This
is a rejection rule.
5. Four
consecutive control observations are on the same side of the mean and exceed mean
1 SD control limit. Reject the run.
6. Ten
consecutive control obser-vationsoccur on the same side of the mean. This is a
rejection rule.
External Quality Control
Internal quality control monitors daily quality
control in a laboratory whereas external quality control is a way to compare
the performance of a laboratory with reference to others. External quality
control is also known as proficiency surveys.
Such proficiency testingprogrammes periodically provide samples of unknown results to participating laboratories. When a laboratory receives such a sample, it must analyse and return the results within a specified period of time for comparison with the results obtained from other laboratories participating in the proficiency survey.
Such proficiency testingprogrammes periodically provide samples of unknown results to participating laboratories. When a laboratory receives such a sample, it must analyse and return the results within a specified period of time for comparison with the results obtained from other laboratories participating in the proficiency survey.
At the
proficiency survey centre, the results from each laboratory are compared to the
expected results or those obtained from a few reference laboratories.
The
comparison may be either with fixed limits or statistically derived limits. For
statistical comparison, the means and standard deviations of all the results
are computed.
The deviation from the mean is expressed as standard deviation indices (SDI) above or below the mean. The SDI is the numerical difference between the individual laboratory's result and the mean, divided by the standard deviation.
The deviation from the mean is expressed as standard deviation indices (SDI) above or below the mean. The SDI is the numerical difference between the individual laboratory's result and the mean, divided by the standard deviation.
A deviation
of more than + 2SDI requires investigative action, whereas a deviation of over
3 SDI is considered unacceptable. The participating laboratories must try their
best to determine the causes of the erroneous results. This will help the
laboratory to improve on the quality of its test results.
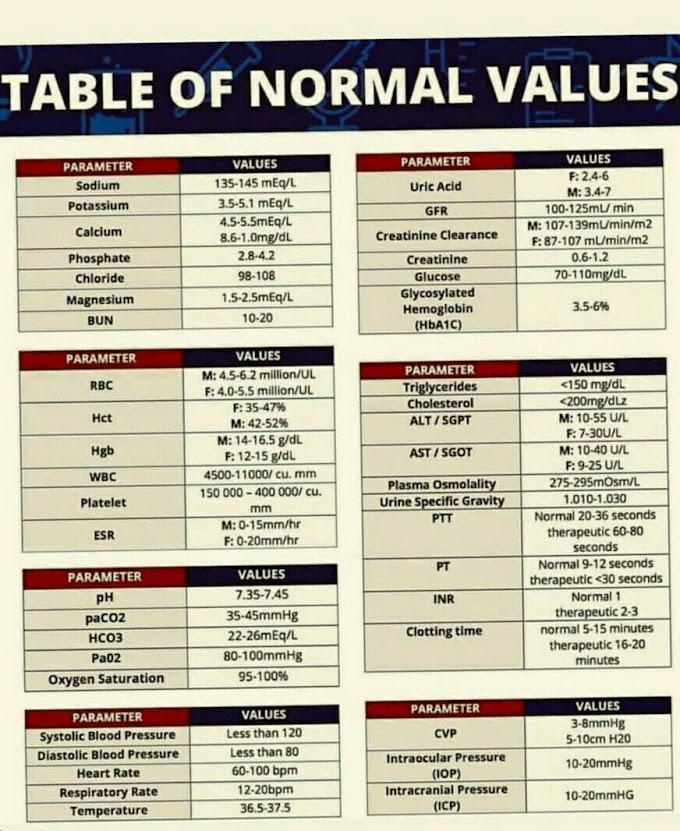
POSTANALYTICAL FACTORS
The postanalytical factors include recording and
transmitting patietn's results to the physician within reasonable time
interval. Once the results reach the physician, he has to decide whether they
fall within normal limits or not.
Therefore, the results should include the reference ranges, critical and technical limits. It is always helpful to check the critical values before reporting them. The reference values which vary with age and sex should be clearly indicated.
Therefore, the results should include the reference ranges, critical and technical limits. It is always helpful to check the critical values before reporting them. The reference values which vary with age and sex should be clearly indicated.
It is of
utmost importance to avoid clerical mistakes in the transmission of clinical
results to the physician. With the use of computer-generated patient reports,
such incidence can be considerably reduced.









If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..