Blood Banking
Blood Transfusion and Compatibility Testing
SELECTION OF A DONOR
COLLECTION OF BLOOD
Blood Containers
Method of Collecting Blood
Anticoagulants and Preservatives Used for Blood Collection
COMPATIBILITY TESTING
Crossmatching
BLOOD TRANSFUSION
Autologous Transfusion
Directed Transfusion
USE OF BLOOD COMPONENTS
FRACTIONS AND DERIVATIVES
Blood Transfusion and Compatibility Testing
Therapeutic
administration of blood and blood products is indicated in many diseases and
other health problems. Loss of blood from the body impairs the ability of the
circulatory system to supply adequate amounts of oxygen to body tissues and
upsets the delicate water and acid-base balance of the body fluids. This can
lead to severe illness and death. Loss of blood may be due to haemorrhage,
excessive destruction of red cells or inability of the body to replenish its
own blood cells.

The technique of replacing a patient's whole blood or its components is known as blood transfusion. The blood used for transfusion should be such that it should not have any harmful effect on the patient. The tests carried out for this purpose are called compatibility tests and are performed on a blood sample of a willing, normal, healthy individual, the donor. The procedures involved in collecting, storing, processing and distributing the blood of potential donors is called blood banking.
SELECTION OF A DONOR
Most healthy
individuals can donate blood without any ill-effects. However, selection and
proper identification of a donor is essential so that the blood collected for
transfusion is safe and beneficial to the patient (recipient). Most blood
donations are voluntary.
Two basic
principles must be kept in mind when the donor is selected:
1. The blood
collection procedure should not be harmful to the donor.
2. The
donor's blood should not be harmful tothe recipient.
The
selection of the blood donor involves a medical history and simple physical
examination (pulse rate, blood pressure), and later, screening for
transfusion-transmissible diseases.
PRE-TRANSFUSION TESTS :
- DONOR'S BLOOD While collecting donor's blood, a small sample of blood should be collected separately for testing before it can be safely transfused into any recipient. The following screening tests must be performed on the donor's blood sample.
Haemoglobin
Concentration :- The
concentration of haemoglobin may be determined by any method described in this
book. It is best to disqualify persons with haemoglobin of less than 12g/100
ml. This rule may be relaxed to permit individuals with 10 g/100 ml haemoglobin
to donate blood in emergencies
Parasites
:- Blood should be screened for blood parasites such as malaria, microfilaria and
trypanosomes, especially in endemic areas.
Tests for Syphilis:- A blood sample positive for syphilis may transmit live
spirochaetes of Treponema pallidum to the recipient. Therefore, screening tests
such as VDRL or RPR should be performed on the donor's sample. The blood should
be discarded if found positive. However, T. pallidum cannot survive for more
than 48-72 hours at 4°C. Hence, the blood stored for more than 72 hours at 4°C
has no risk of transmitting syphilis to the recipient.
Test for Hepatitis B :-Transfusion
of blood from a hepatitis B carrier can result in the transmission of the
disease to the recipient. Therefore the blood sample of the donor must be
screened for the presence of hepatitis B antigen (HBsAg) by one of the various
methods available.
Test for Human Immunodeficiency Virus (HIV) :- Human immunodeficiency virus (HIV), the causative
agent of acquired immunodeficiency syndrome (AIDS) poses the highest risk of
transmission through blood transfusion, and can lead to the fatal disease.
Therefore, every blood donor must be screened for HIV by ELISA or other
screening tests.
Test for Human Immunodeficiency Virus (HIV) :- Human immunodeficiency virus (HIV), the causative
agent of acquired immunodeficiency syndrome (AIDS) poses the highest risk of
transmission through blood transfusion, and can lead to the fatal disease.
Therefore, every blood donor must be screened for HIV by ELISA or other
screening tests.
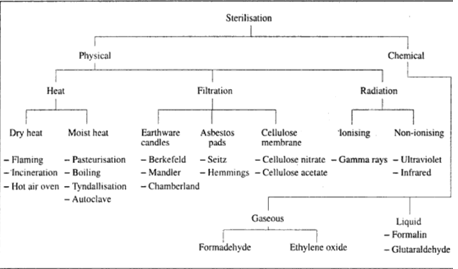
COLLECTION OF BLOOD:
- Blood for transfusion must be collected and handled under strictly sterile conditions to prevent contamination. Plastic blood collection bags are used which contain an anticoagulant sufficient for the amount of blood to be collected. Generally, a combination of citrate and dextrose is used as an anticoagulant. Citrate binds with calcium and prevents activation of the coagulation cascade. Dextrose provides energy for the red blood cells.
The anticoagulant also contains inorganic phosphate buffer to increase the production of energy-rich adenosine triphosphate (ATP) which increases red cell viability. If adenine is added, it increases the survival period of red cells. The two commonly used anticoagulants are citrate phosphate dextrose (CPD) and citrate phosphate dextrose adenine-1 (CPDA-1). When stored at 16°C, CPD anticoagulated blood is approved for 21 days storage while with CPDA-1, blood can be stored for up to 35 days.
Blood Containers:- Plastic
containers of blood have replaced the glass bottles. The plastic bags are more
compact and lighter in storage. They are more flexible and can avoid the hazard
of air embolism. Two or three bags can be connected to each other aseptically
so that components can be separated without contaminating the primary
container.
Method of Collecting Blood:
- While collecting blood, the donor should lie down, and a blood pressure cuff should be used on the arm above the venepuncture site. Under aseptic conditions, make a venepuncture using an 18 gauge needle to obtain a faster flow. The collection bag with anticoagulant should be kept below the level of the arm for gravity flow. Swirl the bag intermittently to bring about mixing of blood with the anticoagulant.
The donor should gently flex the fingers or clench and unclench the fist to assist the flow of blood from the vein. About 420-450 ml of blood can be collected from a donor at a time. When the full amount of blood has been collected, collect the blood into 2 tubes in 5 ml amounts for various screening tests. Seal the venepuncture site on the donor's arm with a plaster to stop the flow of blood. The donor should be allowed to rest for a while and offered a nourishing drink to adjust for the loss of blood.
Proper
labelling of the collecting container is of utmost importance
The label should contain the following information:-
1.Donor identification
number
2.ABO and Rh type
3.The type and volume
of anticoagulant.
4.Volume and name of
the product (e.g.,whole blood, red cells.)
5.Temperature for
storage
6. Date of expiry.
The blood
must be stored in a refrigerator with a constant temperature of 1-6°C. An alarm
should sound if the temperature exceeds the limit. The stored blood should be
inspected daily for colour, turbidity, haemolysis and clot formation, and
should be discarded if there is any evidence of bacterial contamination.
Anticoagulants and Preservatives
Used for Blood Collection:-The
most important factor that affects recovery of red cells after blood storage is
the anticoagulant solution used. The changes in blood on storage are directly
related to the storage time and the type of anticoagulant used. The solutions
commonly in use are both anticoagulants and red cell preservatives, but are
referred to as anticoagulants.
Anticoagulant Citrate Dextrose (ACD):- This solution has been in use and modified for a
number of years since 1918. The anticoagulant contains 100 ml of 2% sodium
citrate and 20 ml of 15% glucose for the preservation of 420 ml of blood. This
anticoagulant is now replaced by CPD and CPDA-1.
Citrate Phosphate
Dextrose (CPD):-This
anticoagulant has a pH higher than that of ACD and is more isotonic. With CPD,
the survival rate of red cells is as good or better than that of ACD, but there
is a remarkable improvement in the red cell function. Therefore, CPD has
replaced ACD as the anticoagulant of choice.
Citrate
Phosphate Dextrose Adenine-1 (CPDA-1) Because the red cell needs ATP as a
source of energy, addition of adenine to CPD helps in the maintenance of high
ATP levels. Adenine is non-toxic and well tolerated by recipients.
The
composition of CPD and CPDA-1 is shown in Table 9.1.
Other Additives and Anticoagulants:- Synthetic enzyme inhibitors are sometimes added to
the anticoagulant to inhibit some enzymes produced by leucocytes which may
cause haemolysis. Ion exchange resins are sometimes used to remove all cations,
including calcium from blood, thus preventing coagulation. Such blood is useful
for plasma production and sometimes for research.
Copostion
of CPD and CPDA and CPDA-1 solution
(for 450 ml of blood)
|
||
Ingredient
|
CPD
|
CPDA-1
|
Trisodium
Citrate(G)
|
1.66
|
1.66
|
Citric
Acid (Mg)
|
206
|
206
|
Dextrose(G)
|
1.61
|
2.01
|
Manobasic
Sodium Phosphate
|
140
|
140
|
Adenine
|
-
|
17.3
|
COMPATIBILITY TESTING:- Before a donor's blood is transfused into a recipient,
there should be no antigens or antibodies in both the donor's blood and
recipient's
blood that would react with each other, resulting in the destruction of red
cells. In other words, there should be no transfusion reaction. The donor's
blood should be compatible with recipient's blood and should give maximum
benefit to the recipient.
Compatibility
testing involves the following:-
1.
ABO and Rh Typing of the Donor and the
Recipient:- ABO and Rh D grouping of
the donor and the recipient blood should be done. Both should belong to the
same ABO group and Rh-D type to be compatible.
The methods of ABO TYPING
Crossmatching:- Crossmatching
is divided into two parts:
1. Major cross match:- It
involves testing donor's red cells with recipient's serum to detect unexpected
antibodies in recipient's serum that will destroy donor's red cells.
2. Minor cross match:- It
tests recipient's red cells with donor's serum in the same way as the major
cross match. These antibodies can also be detected by antibody screening tests.
Major cross match
|
Donor cells + Recipient serum
|
Minor cross match
|
Recipient cell +
Donor serum
|
BLOOD TRANSFUSION:- There are clinical conditions in which therapeutic
replacement of blood is indicated. The potential benefits of transfusion must
always be greater than any potential harm to the patient. The indications for
blood transfusion may be divided into four major categories:
1.
Restoration of oxygen carrying capacity Blood transfusion may be necessary to
restore or maintain the oxygen carrying capacity of blood. The best results are
achieved by transfusion of red blood cells after removing the plasma. If the
plasma is not removed, the increase in total blood volume may result in
circulatory overload.
2.
Maintenance of blood volume in cases of acute blood loss (e.g., post-operative
massive bleeding or bleeding after injury); transfusion of whole blood or
plasma gives good results. However, the best results are obtained by replacing
the lost volume of blood with an electrolyte solution, followed by packed red
cells later.
3.
Maintenance of haemostasis It is sometimes necessary to replace coagulation
factors to maintain haemostasis. Various blood components or derivatives may be
transfused as the situation demands. Examples of such transfusions include
platelet concentrates, fresh frozen plasma, cryoprecipitates and factor VIII
and IX concentrates.
4. Restoration
of leucocyte function The clinical conditions demanding transfusion of
leucocytes do not arise very often, but may be necessary in a granulocytopenic
patient with infection.
Autologous Transfusion:- Transfusion of blood or blood products previously collected
from the same person is called autologous transfusion. Usually such a person
expects to undergo a surgical procedure which may involve loss of blood. The
patient's own blood is preferred because the hazards of immunisation by foreign
material and transmission of disease do not arise. Autologous transfusion may
also be necessary when a person is immunised to some antigens. However,
autologous transfusion is not a common practice.
Directed Transfusion:-This is elective transfusion of blood to a patient with the
blood donated by his family member or a friend. Recently, directed transfusions
have become more common due to the fear of transmission of HIV.
USE OF BLOOD COMPONENTS:-
FRACTIONS AND DERIVATIVES:-Each component of whole blood such
as the formed elements, proteins and electrolytes, has a different and
important function to perform. Therefore, indiscriminate use of whole blood is
not justified when most patients can be effectively treated with one or more of
the components. Optimum use of every blood donation is achieved when each donor
serves more than one patient. It can be accomplished by skilful and intelligent
use of proper blood component or derivative for each indication




If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..