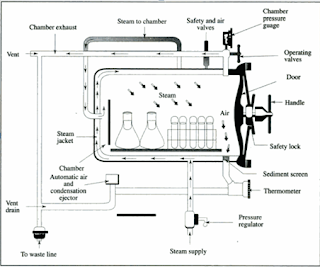
Autoclave:- This is steam above 100°C and it
is the most efficient means of sterilisation. It is routinely used for most
heat-stable materials. An autoclave is used to achieve the high temperature
steam. The boiling point of water is raised by increasing the pressure inside
the autoclave. There are different designs of autoclaves in the market. But
basically the autoclave is a double-walled or jacketed chamber that can
withstand the high pressures required The autoclave has a steam inlet valve and
a steam outlet valve. In addition, it is usually equipped with a safety valve
(set to open at a pre-determined pressure), a temperature gauge and pressure
gauge. The usual sterilization temperature is 121°C at 15 lbs per square inch
(psi) pressure for 15 minutes. Greater the pressure, higher the temperature and
shorter the time of sterilization.
The cycle however
depends on the volume of material to be sterilized and the amount of
contamination expected. It is recommended that large volumes of material such
as culture media or surgical dressings, be dispensed into small volumes or
portions to reduce the time required for sterilization and so decrease the
chance of over cooking or damaging the material.
Although
autoclaving is a highly recommended method of sterilization, its major
drawbacks are that it may cause damage to heat-sensitive materials, and the
load is not dried.
The domestic
pressure cooker is the simplest form of autoclave. The steam displacement
autoclaves which used to be the commonest type, are
becoming
obsolete. A mastery of the operation of all types of autoclaves is essential to
avoid major accidents due to explosion and to prevent over heating of the
material.
Operating an autoclave
The load is
loosely placed in the chamber and the door or lid securely shut. Both the inlet
and outlet valves are open. Steam is introduced into the chamber to force air
out from it, leaving only pure steam. (A rubber tubing attached to the outlet
valve with the end dipped in a bucket of water will stop bubbling when all the
air has been forced out).
Close the
outlet valve, the temperature and pressure will begin to rise. When the desired
temperature and pressure are reached, close the inlet valve. Start to time the
sterilisation cycle to the desired length of time.
This period
of actual sterilisation is known as the 'holding time'. At the end of
sterilisation, open the outlet valve slowly to avoid boiling over of liquid
media. The steam begins to escape and at the same time the temperature and
pressure begins to fall. Never open the autoclave until the pressure is
completely down in order to avoid explosion.
The high vacuum
autoclaves are fast and reliable. Before the admission of steam, 98 per cent of
the air present in the chamber is rapidly removed by electric pump and
sterilisation can proceed without delay. The cycle is short and heat
penetration is efficient. Most of the newest models of autoclaves are fully
automatic. The operator simply loads the autoclave, presses the start buttons
and the autoclave is left unattended to till the cycle is completed.
This table shows the
relationship between time of autoclaving, pressure and temperature.
Pressure,
holding time and tempreture for autoclaviing
|
||||
Gauge pressure(PSI*)
(pressure above atmospheric)
|
Holding time (min)
|
Temperature(*C)
|
||
Pure steam (no air present)
|
50% air-steam mixture
|
No air removed
|
||
5
|
40
|
108
|
94
|
72
|
10
|
30
|
115
|
105
|
72
|
15
|
15
|
121
|
112
|
100
|
20
|
10
|
126
|
118
|
109
|
25
|
5
|
130
|
124
|
115
|
30
|
5
|
134
|
128
|
121
|
Testing the efficiency of the autoclave
There are
several methods of testing whether or not material is adequately sterilised.
The four commonest methods are:
1. Brown's sterilizer
control tubes These are tubes containing an indicator liquid and designed for
steamer, hot air oven and autoclave. The liquid will change from red to green
if the correct temperature time combination has been employed; if not, the
liquid turns a reddish-brown color. The tubes are placed in the area of least
heat penetration.
2.
Biological indicator Filter paper strips impregnated with a sporing organism
such as Bacillus stear other mophilus, is enclosed in an envelope and placed at
the centre of the load to be sterilised. On removal, the strip is cultured in a
suitable medium and incubated at 55°C for one week. No growth indicates proper
sterilisation. This method is good when time factor is not important because
the organism requires long incubation to grow.
3. Autoclave
tapes There are many tapes based on the Bowie-Dick autoclave tape principle of
uniform colour change. The tape indicates the degree of heat penetration. The
tapes have a water resistant gummed side. When sterilisation is adequate and
complete, the tape changes colour uniformly. While the Bowie-Dick tape does not
test for adequate exposure to heat in terms of time and temperature, strips of
tapes may be useful on individual packages as indicators of exposure to heat.
4.
Thermocouples The efficiency of an autoclave is best monitored by means of
thermocouples which are placed within the contents and calibrated to show the
temperature attained.
Sterilisation failure in the autoclave
Sterilisation failures may be due to:
1. Incomplete removal of air from the autoclave. Temperature
of air/steam mixtures at a given pressure is lower than that of pure steam
2. Incorrect methods of packaging.
3. Careless loading into steriliser.
4. Failure to time correctly, the proper period of exposure
(holding time).
5. Attempts to sterilise materials impervious to steam in an
autoclave, e.g., oils.
6. Faulty equipment.
Inspissation: This is the method of coagulating and
further sterilizing culture media that were initially prepared aseptically. The
media should contain a coagulable protein such as serum or egg. It is ideal
therefore for Loeffler's medium or Lowestein Jensen's medium.
The
inspissator is a double walled copper box with water flowing between the two
walls.
The inside
is made in such a way that culture media bottles lie slopped. The temperature
is controlled between 75-80°C thermostatically. Inspissation is carried out for
two hours on each of three consecutive days. A higher temperature may denature
the protein and cause bubbling of the surface of the media.




If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..