BLOOD UREA, Estimation of Blood Urea, by Berthelot Reaction, by Diacetyl Monoxime Method Reagents

UREA - Urea
constitutes almost half the total of the nonprotein nitrogenous substances of
the blood. It is manufactured in the liver from carbon dioxide and ammonia
resulting from the breakdown of amino acids. It is the major excretory product
of protein metabolism.
Urea is carried by the plasma to the kidney where it is
filtered from the plasma by the glomerulus. About 40 % of the urea in the
glomerular filtrate is reabsorbed by the renal tubules. Most of the urea in the
filtrate is excreted in urine while small amounts are excreted through the
gastrointestinal tract and the skin.
Measurements
of urea were initially done on a protein free filtrate of whole blood and so,
early analytical methods were based on measuring the amount of nitrogen.
This
analysis was commonly referred to as Blood Urea Nitrogen (BUN). Though current
methods of urea estimation use whole blood, plasma or serum, the term BUN is
still used by some workers.
The nitrogen
concentration of urea can be converted to urea concentration by multiplying it
by 2.14.
The
concentration of urea nitrogen in mg/dl can be converted to mmol/l of urea by
multiplying by 0.36
Collection of specimens Since urea estimation can be
performed on whole blood, plasma or serum, any routine anticoagulant such as
EDTA can be used except
(i) Sodium
fluoride, because it is an enzyme inhibitor, and therefore, unsuitable for enzyme
methods.
(ii)
Ammonium oxalate, because some methods of estimation of urea depend on the measurement
of ammonia.
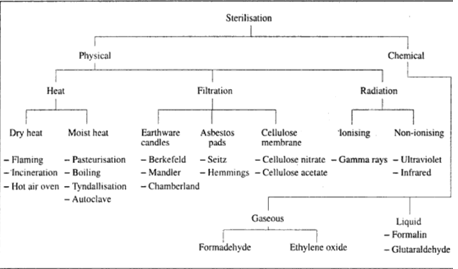
Choice of methods There are three commonly used methods for the estimation of blood urea.
Choice of methods There are three commonly used methods for the estimation of blood urea.
1. Urease method using Nessler's
reaction The enzyme
urease hydrolyses urea to form ammonium carbonate. The aminonium ions produced
are measured by using Nessler's reagent.
2. Urease method using Berthelot
reaction In this
method, the ammonia produced by the action of urease on urea is estimated by
measuring the blue colour of indophenol formed with phenol and hypochlorite.Sodium
nitroprusside is used as a catalyst.
3. Diacetyl monoxime method Urea is heated with diacetyl
monoxime in the presence of a strong acid and an oxidizing agent to form a yellow
diazine derivative. Thiosemicarbazide is added to the mixture to enhance and
stabilise the colour. Methods (2) and (3) will be described in detail.
Estimation of Plasma Urea by
Berthelot Reaction
Reagents
(i) Buffered urease reagent: 1.0g ethylenediaminetetraacetic acid
(EDTA) and 150 mg urease are mixed and shaken in about 70 ml of distilled
water. Adjust pH to 6.5 and make up volume to 100 ml. When stored in a plastic
bottle at 4°C, the reagent is stable for one month.
(ii) Phenol colour reagent Dissolve 50 g analytical grade
phenol in 400 ml distilled water in a volumetric flask. Dissolve separately 250
mg analytical grade sodium nitroprusside in 50 ml of distilled water. Mix the
two solutions together and make the volume up to 1 litre with distilled water.
Store in a dark brown bottle away from light at 4°C. Stability is for about 2
months.
(iii) Alkaline hypochlorite reagent Dissolve 25 g sodium hydroxide in
400 ml distilled water. Dissolve 2.1 g sodium hypochlorite in 100 ml of
distilled water, mix the two solutions and make up the volume to 1 litre.
Storage is same as for the phenol colour reagent.
(iv) Urea standard solution (10
mmol/l) Dissolve 600
mg urea in distilled water and make up to 1 litre. Add a few drops of
chloroform as a
preservative. Store at 4°C.
Method
(a) Set up
test tubes as follows:
Blank
|
Test
|
Standard
|
|
Buffered urease reagent
|
200 ul
|
200 ul
|
200 ul
|
Test plasma
|
20 ul
|
||
Standard
|
20 ul
|
||
Distilled water
|
20 ul
|
(b) Incubate
all tubes at 37°C for 15 min.
(c) Remove
all tubes from the water bath; add 1.0 ml phenol color reagent to each tube.Shake
gently to mix.
(d) Add 1.0
ml hypochlorite reagent to each tube and mix.
(e) Incubate
all tubes at 37°C for 20 minutes.
(f) Remove
all the tubes from water bath; add 5 ml distilled water to each tube.
(g) Read absorbance
of the standard and test Against the blank at 630 nm to 650 nm or with red
filter
Estimation of Blood Urea by Diacetyl
Monoxime Method
Reagents
(I)Sodium tungstate (10 %)
(II) 2/3 N
sulphuric acid Add 2 ml of conc. H2SO4 to about 50 ml distilled water and dilute
up to 100 ml.
(III) Color
reagent
Solution A Dissolve I g diacetyl monoxime, 0.2
g thiosemicarbazide and 9 g sodium chloride in distilled water. Dilute up to 1
litre.
Solution B Add 60 ml conc. H_SO, and 10 ml of 85%
phosphoric acid to 800 ml of distilled water. Dissolve 0.1 g ferric chloride in
the acid mixture; cool and make up to 1 litre.
Reagent mixture Mix solution A and solution B in
equal volumes just before use.
(vi) Urea standard solution (5
mmol/L) Dissolve 300
mg urea in distilled water and make up to 1 litre.
Method
(i) Prepare
protein-free filtrate by mixing 1.0ml of blood, 7.0 ml of distilled water. Mix
and add 1.0 ml of sodium tungstate and 1.0 ml of 2/3 N H 30 Mix and allow to stand
for 5 minutes. Filter or centrifuge.
(ii) Set up
3 tubes as follows:
blank
|
Standard 5.0 ml
|
Test 5.0 ml
|
|
Color reagent
|
5.0 ml
|
5.0 ml
|
5.0ml
|
Distilled water
|
0.5 ml
|
||
Urea standard -
|
0.5 ml
|
||
Specimen(filtrate)
|
0.5 ml
|
(iii) Heat
all the tubes in boiling water bath for exactly 15 minutes.
(iv) Cool and read the absorbance at 520 nm or using
green filter.
Alternatively,
a calibration curve can be prepared
and a graph of absorbance against concentration plotted to determine the amount
of urea in the test sample.
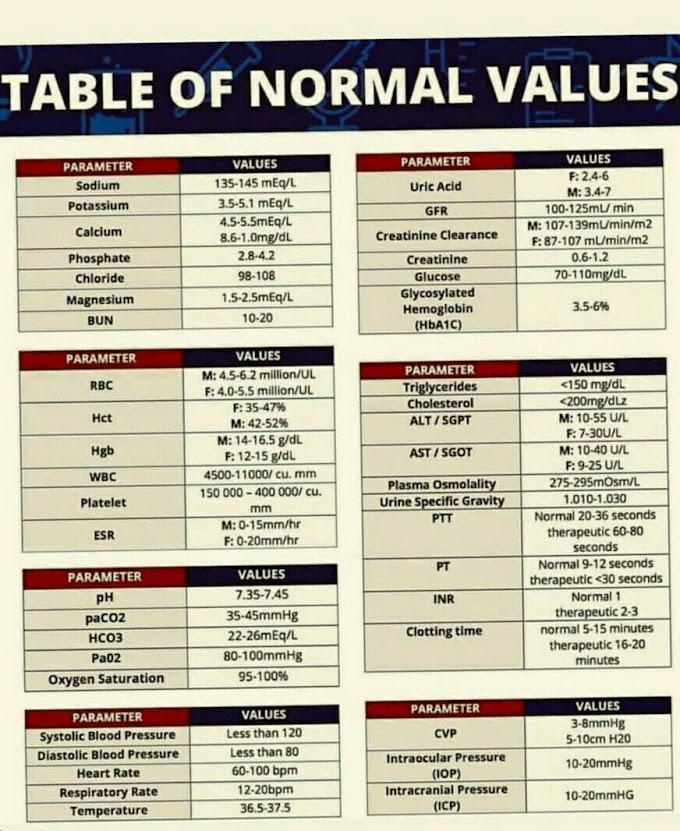
Normal Range of Blood Urea
Adults: 2.5
- 7.0 mmol/L (15 - 40 mg/dl)
Mg/dl of
urea = mmol/L x 6
Note Urea concentration is often expressed
as units of urea nitrogen in blood (BUN) in mg/dl. The molecular weight of urea
is 60. Each molecule of urea contains two nitrogen atoms with a weight of 14 x
2 = 28. Therefore blood urea can be converted to BUN by the factor 28/60, i.e.,
0.467. Conversely, BUN can be converted to urea by multiplying by 60/ 28, i.e.,
2.14.
Interpretation of Blood Urea Results
Blood
normally contains a small amount of urea; and the amount may vary with the
amount of protein in the diet. When the amount of urea in the blood becomes
excessive, the condition is known as uraemia.
This condition is usually a result of impaired kidney function. In the elderly,
the level of urea may be a little higher than normal; and low values may be
found during pregnancy and in full term infants, whereas premature infants may
have slightly higher values than the adult range.
A
considerable rise in the blood NPN level particularly due to urea and
creatinine in a kidney insufficiency is called azotaemia. The cause of azotaemia can be pre-renal, renal, or
post-renal.
Pre-renal azotaemia This is due to poor perfusion of the
kidneys resulting in diminished glomerular filtration. Poor perfusion can be
due to:
(a) Reduced
blood flow to the kidney as a result of shock, dehydration, blood loss or congestive
heart failure.
(b)
Increased protein catabolism as in fever,severe burns, stress, crush injury or
bleeding into soft tissues.
Renal azotaemia This is when urea is retained
primarily due to impaired glomerular filtration which results in acute or
chronic renal disease. The acute state may be due to glomerulonephritis,
nephrotoxic drugs, or renal cortical necrosis. The chronic condition may be due
to glomerulonephritis, pyelonephritis, diabetes mellitus or renal tubular
diseases.
Post-renal azotaemia This is due to the obstruction of
where urea is reabsorbed into circulation. The obstruction can be due to
ureteral destruction by stone, tumour, inflammation or surgical trauma. It can
also be due to obstruction of bladder neck or urethra by enlarged prostate
gland, tumour. inflammation or stones.
Note
Semi-quantitative
methods for the estimation of urea are available. One of such methods is the
Urastrat which is based on a test strip coated with the urease reagent. The
methods are useful in emergencies, small clinics or as screening procedures.
Apart from
the measurement of the amount of urea in the blood, there are many methods for
determining the impairment of the kidneys. But because most of the methods are
cumbersome, they are not used routinely.
Determination of Urine Urea
Collect a 24
hour specimen of urine, which is preserved with thymol or toluene. Dilute the
urine 1:20 and determine the urea concentration of the diluted urine using any
method described for blood urea. Multiply the results by the dilution factor (x
20) to obtain the concentration in mmol/L or g/dl.
Normal range 250-600 mmol/L or 15-35 g/dl
Urea clearance test The average urea clearance over a 24
hour period can be determined by collecting a 24 hour urine specimen and taking
a blood sample around mid-day. Determine the plasma and urine urea
concentrations and calculate average urea clearance in the same manner as the
creatinine clearance (see below).
Normal range 40-65 ml/min. It may fall to about
10ml/min during renal failure and may reach to 2-3 ml/min in terminal cases.
Note
Urea
clearance test is no longer used as a measure of glomerular filtration rate
(GFR) because it underestimates GFR.








If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..