Safety in the Laboratory
The practice
of medical laboratory science is associated with hazards and accidents. The
laboratory worker is very much at risk of acquiring transmissible diseases
through contact with patients or handling of clinical specimens. Though
accidents do occur in the best of laboratories, a poorly designed and
overcrowded laboratory has the increased possibility of hazards and accidents.
It should be noted however, that bad laboratory practices are the major causes
of laboratory accidents. It follows, therefore, that the laboratory should be
manned by well-trained, dedicated and meticulous staff. Every laboratory must
have an appropriate code of safe laboratory practice. It is important that all
accidents be promptly reported to the safety officer or to the officer
in-charge of the laboratory
The hazards
and accidents in the laboratory may be discussed under the following areas:
1. Infection
2. Burns
3. Cuts and
pricks
4. Hazards
of toxic chemicals
5. Electric shocks
5. Electric shocks
1. Infection
-Infections in the laboratory can occur in different ways, but the commonest
causes are:
1.
Inhalation of pathogens in air-borne droplets (aerosols) which are released
during breakage or spilling of infectious fluids, centrifuging, dispensing or
pipetting of infectious materials; and snap-opening and closing of specimen
containers.
2. Ingestion
of pathogens from contaminated food or fingers.
3. Ingestion
of pathogens by mouth-pipetting.
4. Pathogens
finding their way into the body through needle pricks, cuts, scratches,
insect-bites, sores or skin lesions.
2. Burns :- Burns
sustained in the laboratory may be caused by:
1.
Inflammable substances catching fire
2. Fires
from bunsen burners, spirit lamps or from faulty or overloaded electric
circuits
3. Swallowing of corrosive substances during pipetting
or spilling, such substances on the skin.
3. Cuts and
Pricks- Cuts and
pricks may result from:
1. Edges of
broken glasswares.
2. Edge of a
knife.
3. Accidental
pricking with needle or any other sharp instrument
4. Walking on glass chippings.
4. Hazards
of Toxic Chemicals:-Hazards due
to toxic chemicals result from:
1.
Inhalation of fumes of toxic chemicals.
2. Swallowing or ingesting toxic chemicals during
mouth pipetting.
3. Skin
contact with toxic chemicals.
5. Electric
shocks:-
Electric
shocks, usually due to ignorance or carelessness can be caused by:
1. Faulty
electrical circuits.
2. Incorrect
installation of equipment.
3. Touching
exposed live wires.
SAFETY PRECAUTIONS AGAINST INFECTION
All
specimens arriving in the laboratory should be regarded as being potentially
pathogenic. It is a very wrong notion to think that only specimens meant for
bacteriological investigation are infectious.
A specimen of cerebro-spinal fluid sent for glucose estimation may be a part of the same specimen sent for bacterial meningitis investigation. The same is true of a specimen of blood sent for hemoglobin or packed cell volume measurement which may contain infectious microorganisms.
The laboratory worker, must therefore, observe some "dos" and "don'ts" in order to prevent laboratory acquired infections. Some of the rules for the laboratory worker are :
A specimen of cerebro-spinal fluid sent for glucose estimation may be a part of the same specimen sent for bacterial meningitis investigation. The same is true of a specimen of blood sent for hemoglobin or packed cell volume measurement which may contain infectious microorganisms.
The laboratory worker, must therefore, observe some "dos" and "don'ts" in order to prevent laboratory acquired infections. Some of the rules for the laboratory worker are :
1. He/she
should wear protective clothing (laboratory coats/gowns) over normal
clothing:
preferably, wear closed shoes and not walk barefooted in the laboratory.
2. All
specimens and infected materials should be handled with care.
3. He/she
should avoid eating, drinking or chewing gum in the laboratory.
4. He/she
should refrain from smoking in the working zone of the laboratory and also
refrain from applying cosmetics in the laboratory
5. Nothing
should be pipette with the mouth. Gummed labels should not be licked neither, should
pens or pencils be put in the mouth, or stuck in the hair.
6.
Protective gloves or plastic aprons should be worn when collecting blood sample
for hepatitis, AIDS or viral hemorrhagic fever investigations.
7. Used
needle should be inserted back into its guard immediately after use. But due to
the increased awareness of the risks of infection from needle pricks, it is no
longer advisable to recap used needles. Instead, "Sharp safe"
containers should be made available for immediate disposal of used needles. The
containers are finally incinerated.
8. When handling specimens or culture containing
highly infectious pathogens gloves
should be worn.
9. Process
specimens or cultures containing highly infectious pathogens in the safety cabinet.
10. Any
cuts, insect bites, open sore or wounds should be covered with water-proof adhesive
dressing.
11. Finger
nails should be kept short.
12. All
infected or contaminated materials should be disinfected before disposal.
13. There
should be a jar of disinfectant on each bench at the start of the day's work.
The disinfectant must be changed everyday.
14. In case
of any spillage, disinfectant solution should be poured to cover the spilled material
and left for
15 minutes
before cleaning up.
15. Infected glassware should be disinfected by soaking overnight in hypochlorite solution
and cleaning thoroughly under running tap water. At the end of the day, all the
work benches should be cleaned with disinfectant.
17. Before
leaving the laboratory for any length of time hands should be washed with soap
and water thoroughly.
MAJOR CAUSES OF LABORATORY HAZARDS
The
prevention of common accidents is very well documented in many laboratory
manuals. It is very necessary that all members of the laboratory staff are
conversant with the nature of these hazards and their prevention. The most
common accidents even in the smallest laboratories are mainly due to the
following:
1. Dangerous
chemicals
2. Fire
3. Careless
use of laboratory equipment,
Dangerous
chemicals and reagents.
1. Dangerous
Chemicals
Dangerous
chemicals are used in the laboratories either directly or incorporated into
reagents and stains. These dangerous chemicals include the highly flammable
ones like ether or alcohols, highly corrosive ones like phenol or sulphuric
acid, toxic ones like formaldehyde solution, carcinogenic ones like benzidine
or explosive ones like picric acid
To minimise
accidents caused by the chemicals, it is mandatory for manufacturers to label
dangerous chemicals with hazard symbols and supply simple instructions for use
and storage.
It is also important to label clearly those reagents prepared from the dangerous chemicals. The labelling should include the nature and strength of the reagents or solutions, date of preparation, expiry date and any other safety warning applicable. It is advisable that only chemicals required for daily use should be kept in the main laboratory, and the others in the store room. It is also recommended to examine the containers periodically to detect in time any possible build up of pressure which may cause the container to burst.
It is also important to label clearly those reagents prepared from the dangerous chemicals. The labelling should include the nature and strength of the reagents or solutions, date of preparation, expiry date and any other safety warning applicable. It is advisable that only chemicals required for daily use should be kept in the main laboratory, and the others in the store room. It is also recommended to examine the containers periodically to detect in time any possible build up of pressure which may cause the container to burst.
The accepted
hazard symbols are shown in Fig. 2.1.
Store rooms
in which bulk stocks of chemicals are kept should be designed to reduce the
risk of fire. Fire extinguishers should be placed just outside the store rooms.
They should also be well ventilated and adequately lit. Radioactive substances require proper supervision of their storage as provided for by the law.
They should also be well ventilated and adequately lit. Radioactive substances require proper supervision of their storage as provided for by the law.
The
prevention of hazards and accidents due to dangerous chemicals and reagents
lies mainly in the careful observance of safety precautions during handling and
storage.
Flammable
chemicals These chemicals should be stored in fire-proof metal boxes at ground
level preferably in an outside, cool, locked store.
Only small amounts of flammable chemicals should be left inside the laboratory.
A container of flammable liquid should never be opened near an open flame. A bottle of ether should be opened at least three metres away from naked flame. "No smoking" rule must be enforced in the laboratory at all times.
Only small amounts of flammable chemicals should be left inside the laboratory.
A container of flammable liquid should never be opened near an open flame. A bottle of ether should be opened at least three metres away from naked flame. "No smoking" rule must be enforced in the laboratory at all times.
Corrosive
substances Corrosive chemicals such as strong acids (e.g., concentrated
sulphuric or nitric acid) and caustic alkalis (e.g., sodium hydroxide,
potassium hydroxide) should be stored at the floor level. Never mouth pipette a
corrosive liquid; always use an automatic pipetter or dispenser.
Eyes must be
protected from the fumes of corrosive substances. When mixing, acid should
always be added slowly to water, but never the reverse. In case of spillage,
wear protective footwear when cleaning up the area. Wash acid and alkali burns
under a free stream of running cold water. Toxic and irritating chemicals
Toxic
chemicals are equally irritating and can cause death or serious ill-health if
swallowed, inhaled or allowed to come in contact with the skin. Some of these
chemicals cause irritation of the skin and mucous membranes. Highly toxic
chemicals such as potassium cyanide should be kept in locked cupboards. Wear
protective gloves when handling a toxic substance
.
.
Always wash
hands immediately after using a toxic or harmful chemical. Chemicals such as
formaldehyde or ammonia with an irritating or harmful vapour should be used in
a fume cupboard or safety cabinet. Always use an automatic pipetter or
dispenser to measure a toxic chemical.
Carcinogenic chemicals These chemicals are capable of causing cancer when inhaled, or ingested or when they come in contact with the skin.
Carcinogenic chemicals These chemicals are capable of causing cancer when inhaled, or ingested or when they come in contact with the skin.
The chance
of being affected depends on the length and frequency of exposure to, and
concentration of the chemical. The carcinogenic substance should be stored in a
closed container. Wear protective gloves and a face mask when handling a
carcinogen. Wash everything used in handling the carcinogen thoroughly in cold
water.
Explosive
chemicals An explosive chemical can explode as a result of heat, flame or
friction. Chemicals such as picric acid should be stored under water. Never leave
such an explosive chemical in a dry state. Radioactive chemicals All areas
where radioactive
materials are stored or used must be posted with caution signs.
Traffic in this area should be restricted to essential personnel only. Decontamination of laboratory equipment, glassware and work areas should be routinely done on a regular basis.
Traffic in this area should be restricted to essential personnel only. Decontamination of laboratory equipment, glassware and work areas should be routinely done on a regular basis.
Note
Only
properly trained personnel are allowed to work with radioactive chemicals; such
persons must be regularly monitored to ensure that the maximally possible dose
of radiation is not exceeded.
REPORTING ACCIDENTS
Any accident
in the laboratory involving personal injuries, even minor ones, should be
immediately reported to the person in-charge of the laboratory. This first
report of injury should be followed by an accident investigation report.
The injury report should contain the name of the injured person, time and place of injury, and nature of injury. The investigation report should include the information on the injured person, an account of the accident, the cause of the accident, the nature of the injury and the actions to be taken to prevent a recurrence.
The injury report should contain the name of the injured person, time and place of injury, and nature of injury. The investigation report should include the information on the injured person, an account of the accident, the cause of the accident, the nature of the injury and the actions to be taken to prevent a recurrence.
Most
accidents occur due to two main causes:
1.
Environmental factors These include unsafe conditions such as inadequate
safeguards, use of improper or defective equipment, hazards associated with the
location or poor housekeeping.
2. Personal
factors Personal factors are improper laboratory attire, lack of skills or
knowl edge, specific physical or mental condition and at titude to work
Safety Equipment
Safety
equipment has been developed specifically for use in the clinical laboratory.
Equipment for accident prevention and control includes fire extinguishers, fire
blankets, first-aid supplies, safety showers, eye-wash stations, spill kits and
hazard labeling systems.
For personal
protection, safety glasses or protective work shields should be used to protect
the eyes and face from splash and impact. Gloves and rubberised sleeves or
gowns protect the hands, arms or body. Closed footwear should be used.
BIOSAFETY IN
CLINICAL LABORATORY
Bio safety involves safe handling and disposal of hazardous biological materials in the
laboratory. These materials consist of infectious agents themselves as well as
substances actually or potentially contaminated with them.
A large number of laboratory workers handle such materials as part of their daily routine. These workers should be aware of the risks of infection while handling the specimens, and must know appropriate laboratory practices to avoid these risks.
A large number of laboratory workers handle such materials as part of their daily routine. These workers should be aware of the risks of infection while handling the specimens, and must know appropriate laboratory practices to avoid these risks.
In 1984, the
Centre for disease Control (CDC) and the National Institute of Health (NIH) issued
guidelines for use in working with infectious agents in the laboratory. It has
been recommended that all specimens from all patients should be considered
potentially infectious.
The approach is referred to as "universal
precautions" and eliminates the need to identify the patients infected
with human immunodeficiency virus (HIV) or other blood borne pathogens.
Infectious agents such as HIV have been isolated from blood, semen, saliva, urine, cerebrospinal fluid, tears, breast milk, cervical secretions and tissues of infected persons.
A laboratory worker should consider skin (especially when scratches, cuts, abrasions or other lesions are present) and mucous membranes of the eye, nose, mouth and respiratory tract as potential pathways for entry of infectious agents.
Infectious agents such as HIV have been isolated from blood, semen, saliva, urine, cerebrospinal fluid, tears, breast milk, cervical secretions and tissues of infected persons.
A laboratory worker should consider skin (especially when scratches, cuts, abrasions or other lesions are present) and mucous membranes of the eye, nose, mouth and respiratory tract as potential pathways for entry of infectious agents.
Needles and other sharp instruments must be
carefully handled and properly discarded. Spilling and splashing of infected
materials should be avoided.
Summary of "Universal Precautions for Laboratories" by CDC
1. Universal
precautions should apply to blood and all body fluids containing visible blood,
semen, vaginal secretions, tissues, cerebrospinal fluid, pleural fluid,
peritoneal fluid, pericardial fluid, synovial fluid and amniotic fluid.
2.
Laboratory workers should use protective barriers appropriate for the
laboratory procedure and the type and extent of exposure expected. All persons
processing blood should wear gloves and laboratory coats; and these should be
removed before leaving the laboratory. Biological safety barriers should be used
wherever necessary.
3. Hands
should be washed immediately when contaminated with blood or other body fluids,
after removing gloves, and after completing laboratory activities.
4. Use of needles and syringes should be minimised. They should be used in situations in which there is no alternative. If used, needles should not be recapped, or bent or broken by hand. After use, needles and other sharp instruments should be placed in a 'sharp-safe' puncture-resistant container for disposal.
5. Specimens of blood should be placed in strong, leak-proof containers during transport.
6. Mouth pipetting must not be performed in the laboratory. Mechanical pipetting devices should be used.
7.
Contaminated materials used in the laboratory should be decontaminated
appropriately before reprocessing or disposal.
8. Laboratory work surfaces should be cleaned and decontaminated with appropriate disinfectant after a blood or body fluid spill and at the end of day's work.
Specific Precautions against Hepatitis B Virus (HBV) and Human Immunodeficiency Virus (HIV) Infections
An accidental injury such as needle-stick injury to the worker with infectious material from a known case of HBV or HIV infection should be immediately followed by the following.
For HBV infection HB vaccine and HB immunoglobulin, test for HBV antibody.
For HIV infection Treatment with zidovudine (AZT), test for HIV antibody.
After that a
follow up at 1.5, 3 and 6 months.
Containment
Contamination with infectious material is the greatest hazard in clinical microbiology laboratories. Clinical laboratory personnel, including cleaners, clerical staff and maintenance personnel, and also any visitor who enters the laboratory, are subject to the risk of laboratory infection. For this reason, there is growing concern about safe practices, procedures and facilities in the laboratories. Adherence to the principles of biosafety contributes to a healthier and safer work environment for the laboratory staff and the surrounding community
.
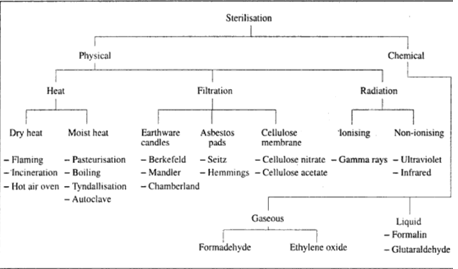
The term
containment essentially describes safe methods for managing infectious agents
in the laboratory environment where they are being handled or maintained. The
purpose of containment is to reduce exposure of laboratory workers and other
persons to, and to prevent escape into the outside environment of potentially
hazardous agents.
The three elements of containment include:
The three elements of containment include:
1.
Laboratory practice and technique
2. Safety equipment (Primary barriers)
2. Safety equipment (Primary barriers)
3. Facility design
(Secondary barriers)
1.
Laboratory practice and technique Each laboratory should adopt or develop a
biosafety manual which specifies practices and procedures designed to minimise
or eliminate risks. Persons working with infected materials or infectious
agents must adhere to standard microbiological practices and techniques
required for safe handling of such materials. They should be aware of the
potential hazards of improperly packed, broken or leaking packages, and of the
proper methods for their handling and decontamination. The use of vaccines may
provide an increased level of personal protection.
2. Safety
equipment (Primary barriers) Safety equipment includes biological safety
cabinets and use of enclosed containers designed to prevent formation of
aerosols. There are three types of biological safety cabinets used in
microbiology laboratory (Class I, II, and III). These are described in
Microbiology Section of this book. Safety equipment also includes items used
for personal protection such as gloves, coats, gowns, face shields and safety
glasses, and should be used wherever appropriate.
3. Facility
design (Secondary barriers) The design of the laboratory facility depends on
the laboratory's function and the risk of transmission of the infectious agents
being manipulated. The basic facility design may include separation of
laboratory work area from public access, availability of decontamination
facility such as autoclave, and handwashing facilities. As the risk of
transmission of more hazardous agents increases, special design features such
as specialised ventilation systems, airlocks at laboratory entrances, or
separate buildings or modules for specialised work area may be provided.
Biosafety
Levels
There are
four biosafety levels (BSL) to which in fectious agents are assigned on the
basis of their virulence.
Each biosafety level has guidelines for appropriate containment level which
consist of combinations of laboratory practices and techniques, safety
equipment and laboratory equipment. Table 2.1 details the biosafety levels for
infectious agents recommended by the CDC. Biosafety level
1 Biosafety level 1 is for laboratories in which work is done with well-defined and characterized organisms not known to cause disease in healthy adult humans. It includes certain non-virulent strains of Escherichia coli (such as K-12) and Bacillus subtilis. This BSL involves standard microbiological practices and safety equipment is not needed.
Biosafety
level
2 Biosafety level 2 is the minimum level for clinical laboratories in which work is done with moderate risk agents present in the community and associated with human disease of varying severity. Hepatitis B virus, Salmonella species and Toxoplasma species are some examples of microorganisms assigned to this containment level. BSL 2 includes good microbiological practice, limited access to the work area, decontamination of all infectious wastes, use of protective gloves, and a biological safety cabinet of Class I or II for use in procedures that may create aerosols. In other circumstances, these agents can be used safely in activities conducted on open bench
.
2 Biosafety level 2 is the minimum level for clinical laboratories in which work is done with moderate risk agents present in the community and associated with human disease of varying severity. Hepatitis B virus, Salmonella species and Toxoplasma species are some examples of microorganisms assigned to this containment level. BSL 2 includes good microbiological practice, limited access to the work area, decontamination of all infectious wastes, use of protective gloves, and a biological safety cabinet of Class I or II for use in procedures that may create aerosols. In other circumstances, these agents can be used safely in activities conducted on open bench
.
Biosafety
level 3 Biosafety level 3 is necessary in the laboratories in which work is
done with agents that are associated with risk of serious or fatal aerosol
infection. Mycobacterium tuberculosis, Brucella species, Yersinia pestis.
Coccidioides immitis, and a wide variety of viruses including human
immunodeficiency virus (HIV) are included in BSL 3. At this containment level,
more emphasis is placed on primary and secondary barriers to protect personnel,
community and environment from exposure to potentially infectious aerosols.
Properly maintained biological safety cabinets (Class II and III) should be
used for all manipulations of infectious materials.
Biosafety
level 4 Biosafety level 4 practices, safety equipment and facilities as
indicated in Table 2.1 are applicable to work with dangerous and exotic agents
which pose a high risk of life threatening disease to individuals. Maximum
containment and decontamination procedures are used in containment level 4,
which is usually found only in reference and research laboratories. Only a few
viruses such as Lassa, Ebola and Marburg are classified in BSL 4.
BIOSAFETY PROGRAMME
Responsibility for Safety
Both the
employer and the employee share the responsibility for safety in a clinical
laboratory. The employer has moral and legal obligations to provide a safe
workplace. The employee also should be aware of his role in his own safety and
the safety of his co-workers. There should be a laboratory safety programme
with clearly stated responsibilities of the management and the employees.
Responsibilities of the Management
1.
Development of a safety programme to establish laboratory work methods and
safety policies.
2.
Establishment of a safe workplace, including the provision of proper safety
equipment and personal protective equipment where needed.
3.
Establishment of appropriate on-the-job training for the employees so that they
are aware of proper safety practices, and provision of supervision and guidance
to laboratory workers whenever necessary.
4.
Development and implementation of an effective infection control programme.
Responsibilities
of the Employee
1. Knowledge
and compliance with the established laboratory work practices.
2. Conduct
of safe work practices and utilisation of personal protective equipment.
Most
accidents occur due to two main causes:
1.
Environmental factors These include unsafe conditions such as inadequate
safeguards, use of improper or defective equipment, hazards associated with the
location or poor housekeeping.
2. Personal
factors Personal factors are improper laboratory attire, lack of skills or
knowl edge, specific physical or mental condition and at titude to work
Safety Equipment
Safety
equipment has been developed specifically for use in the clinical laboratory.
Equipment for accident prevention and control includes fire extinguishers, fire
blankets, first-aid supplies, safety showers, eye-wash stations, spill kits and
hazard labelling systems.
For personal
protection, safety glasses or protective work shields should be used to protect
the eyes and face from splash and impact. Gloves and rubberised sleeves or
gowns protect the hands, arms or body. Closed footwear should be used.
3. Proper
notification of unsafe conditions to the immediate supervisor.
4. Positive
attitude towards training, facilities, co-workers and supervisors.
Health care
facilities such as hospitals and clinical laboratories generate large amount of
waste material that can prove harmful to the community at large if proper
precautions are not taken for its disposal. This waste is collectively called
"medical waste". Medical waste is defined as special waste from
health care facilities that may transmit infectious diseases. It comprises
articles and products such as
1. Blood and
blood products
2.
Microbiological waste
3.
Pathological waste
4. Sharp instruments such as syringe needles
5. Disposable
equipment such as syringes,tongue depressors, intravenous bags. It is important
to identify potentially infectious waste so that it can be separated from the
main waste stream and disposed off in a safe way.
1. Handling
of Medical Waste
Proper
handling of medical waste involves the assurance that it is placed in
designated containers and decontaminated in time using proper technology.
General guidelines are:
1. All
medical waste should be placed in a leakproof container which is puncture resistant
and rigid enough to avoid leakage or puncture during transportation. The
containers should be clearly labelled with biohazard symbol.
2. All sharp
instruments such as needles, blades and glass objects should be placed in
special puncture resistant (sharpsafe) containers before placing them in the
disposal bag. Needles should not be transported, recapped, bent or broken by
hand.
3. Waste
should only be handled by those who have been trained in proper handling.
4. All the
medical waste must be disposed off by one of the recommended procedures.
5. If
contaminated waste needs to be stored for any length of time before disposal,
it should be placed in a secured area accessible only to those who are
responsible for its disposal.
Methods of waste disposal The approved methods
for disposal of medical waste include:
1.
Incineration.
2. Steam sterilisation followed by removal to landfill.
3.
Inactivation by heat.
4. Chemical
inactivation or oxidation.
5. Encapsulation in a solid matrix.
2. Fire
Fire can
break out in any laboratory if proper safety precautions are not observed. It
is essential that the laboratory staff is properly educated on the causes and
controls of fires. The fire can be caused by:
(a) Ordinary
combustibles such as paper, wood, etc.
(b) Flammable
liquids such as ether, alcohols, etc.
(c) Gases
such as methane
(d) Metals
such as magnesium, potassium, etc.
(e) Faulty
electric circuits or appliances
Precautionary measures against fire
1. The
laboratory staff should have fire drills from time to time.
2. Fire
extinguishers for all types of fire must be kept handy in the laboratory. The
fire extinguishers in common use are water, foam, dry powder, carbon dioxide
and halogen. (The use of halogen may be discontinued due to its adverse effect
on the atmospheric ozone layer.)
3. Fire
extinguishers should always be free and in good working condition.
4. Keep
flammable liquids away from naked flame.
5. In case
of a major fire, someone should be delegated to take charge of fighting the
fire. The practice of regular fire drills will help minimize casualties.
3. Equipment or Instrument-related Accidents
Accidents
occur as a result of incorrect positioning, installation and wrong use of
equipment. Poor maintenance and irregular servicing of equipments also lead to
accidents.
It is
important to position the equipment in such a way that safety and convenience
afe given priority over other considerations. It is therefore essential not to
overcrowd the bench with too many equipments. Equipment like refrigerators and
freezers should not be placed too close to the wall.







If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..