OSMOTIC FRAGILITY TEST AND PROCEDURE
PROCEDURE FOR OSMOTIC FRAGILITY TEST
OSMOTIC FRAGILITY TEST PROCEDURE
TECHNIQUE FOR OSMOTIC FRAGILITY TEST
OSMOTIC FRAGILITY TEST INTERPRETATION
OSMOTIC FRAGILITY TEST
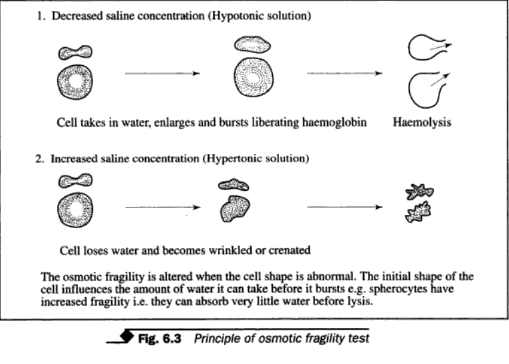
This test
may be required to investigate haemolytic anaemias due to red cell membrane
defect, e.g. spherocytosis. Principle The test determines the resistance of red
cells to haemolysis in various concentrations of hypotonic saline solutions
(Fig. 6.3). The ability of erythrocytes to absorb water without lysis depends
on the ratio of volume to surface area of the cells. In the normal red cells,
the volume may increase up to 70 % before lysis can occur. Spherocytes have
reduced surface to volume ratio and therefore absorb less water.
 |
| principal of osmotic fragility test |
Specimen
Serum
Technique
(i) Mix one
drop of patient's serum with one drop of well mixed latex suspension coated
with DNP, on a slide.
(ii) Rotate
for one minute and examine for agglutination.
(iii) Run a
known positive control in the same way along with the test. Result
Agglutination appearing within one minute indicates a positive test.
Reagents
1. The stock
solution of sodium chloride osmotically equivalent to 10 % is prepared as
follows.
Sodium
chloride 90gm
Disodium
hydrogen phosphate 13.65 g
Sodium
dihydrogen phosphate 2.34 g
Distilled
water 1 liter
Specimen
Heparinised venous blood or defibrinated blood should be used. Oxalated, citrated or EDTA blood should be avoided because additional salts may interfere with the test. The test should be carried out immediately. If delay is expected, the blood should be preserved at 4°C and the test performed within six hours.Technique
(i) Dilute the stock solution of sodium chloride 1:10 with distilled water to
obtain a 1 % solution.
(ii) take 12
tubes and prepare dilutions as follows:
(ii)
take 12 tubes and prepare dilutions as follows:
|
|||
Table
no
|
1% nacl (ML)
|
Distilled water(ml)
|
Final concentration
|
1
|
4.5
|
0.5
|
0.9
|
2
|
3.75
|
1.25
|
0.75
|
3
|
3.75
|
1.75
|
0.65
|
4
|
3.25
|
2
|
0.6
|
5
|
2.75
|
2.25
|
0.55
|
6
|
2.5
|
2.5
|
0.5
|
7
|
2.25
|
2.75
|
0.45
|
8
|
2
|
3
|
0.4
|
9
|
1.75
|
3.25
|
0.35
|
10
|
1.5
|
3.5
|
0.3
|
11
|
1
|
4
|
0.2
|
12
|
0.5
|
4.5
|
0.1
|
(iii) Add
0.05 ml of the blood to each of the tubes and mix immediately by gently inverting
several times.
(iv) A blood
sample from a normal individual is run in parallel as a control.
(v) Stand at
room temperature (18-20°C) for 30 minutes.
(vi) Remix
and centrifuge.
(vii) The
amount of lysis in each tube is determined colorimetrically using a green
filter, at 540 nm. The first tube in the series serves as a blank (0 % lysis)
as it contains 0.9 %. isotonic saline. The 12th tube containing 0.1 % saline
serves as 100 % lysis since this gives complete lysis.
Calculation
Plot a graph
of % lysis against concentration of sodium chloride (Fig 6.4) Record the
results as
1. Complete
lysis or maximum resistance as the highest concentration of saline showing
complete lysis.
2. Initial
lysis or minimum resistance as highest concentration of saline in which lysis
appears to be just detectable.
Normal
range of osmotic fragility is indicated as shown below:
|
|
Concentration of sodium chloride
|
% Lysis
|
0.1
|
100
|
0.2
|
100
|
0.3
|
97-100
|
0.35
|
90-99
|
0.45
|
50-90
|
0.5
|
5-45
|
0.55
|
0-6
|
0.6
|
0
|
0.65
|
0
|
0.7
|
0
|
0.75
|
0
|
0.8
|
0
|
0.85
|
0
|
The normal
fragility curve should fall in the shaded area shown in the graph (Fig. 6.4).
Alternatively,
the osmotic fragility may be expressed as the concentration of NaCl causing 50
% haemolysis, Mean Corpuscular Fragility
(MCF), from the graph. The normal range for MCF is 0.4 to 0.45 g/100 ml.
Note The osmotic fragility is increased
when the lysis starts at a concentration higher than 0.5 % and is decreased
when 100 % lysis starts at a concentration lower than 0.3 %.
Interpretation Various haematological disorders show
characteristic changes in osmotic fragil. ity. Osmotic fragility is increased
(i.e. resistance reduced) in hereditary spherocytosis, in ABO haemolytic
disease, and haemolytic disease of the new-born. It is reduced (i.e. resistance
increased) in thalassaemia, iron deficiency anaemia, liver disease and
splenomegaly.








If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..