FIBRINOLYSIS
The process of removing unwanted, insoluble deposits formed
as a result of coagulation is called fibrinolysis. It is a physiological
process in which a fibrin clot is broken down by enzymes into soluble
fragments. The fibrinolytic system involves conversion of a plasma proenzyme
plasminogen into plasmin digest fibrin and breaks it into soluble fragments.
Plasmin is also capable of breaking down fibrinogen, factor
V and factor VII in the presence of plasminogen activators. These activators
are present in the largest quantities in the endothelial cells of capillaries.
They are also found in small amounts in plasma and in lysosomes of most body cells.
The endothelial cells also secrete another important
plasminogen activator called tissue-type plasminogen activator (t-PA). The t-PA
does not circulate in an inactive form like other activators. It is secreted in
large amounts in an active form by the endothelial cells in response to various
stimuli. When released, it continuously interacts with plasminogen activator
inhibitor (PAI) forming an inactive complex. High levels of t-PA are associated
with bleeding disorders. PAI is present in small amounts in plasma and in much
larger amounts in platelets. High PAI levels are seen in sepsis, in pregnancy
and are associated with thrombotic activity.
Increased levels of plasminogen are observed in acute
bacterial infections, inflammatory conditions, myocardial infarction,
thrombophlebitis, pregnancy and after long term use of oral contraceptives.
DISORDERS OF BLOOD
COAGULATION The common causes of coagulation disorders include deficiencies
of coagulation factors, inhibitors of coagulation factors and defects in
platelet function. The disorders may be hereditary or acquired. Some commonly
occurring disorders are mentioned below.
I Inherited Disorders
1. Haemophilia A
(classical haemophilia)
Haemophilia A is the most commonly inherited disorder of the
coagulation factors. The frequency of the disease is approximately 1:25,000 and
males are primarily affected. This disorder occurs due to the deficiency of a small
subunit of the factor VIII molecule called factor VIII antigen (VIII:Ag). This
deficiency is carried on the X chromosome.
Therefore, haemophilia A occurs almost exclusively in males
and is very rare in females. Clinically, classical haemophilia occurs along
with haemorrhage. Such haemorrhages can occur both internally and externally.
Bleeding into joints and muscles is typical. Other symptoms include excessive
bleeding after surgery or major trauma, and even after superficial abrasions.
Bleeding may also occur through the nose, mouth, eyes and gastrointestinal
tract. Severe bleeding may lead to a rapidly progressive normocytic anaemia.
Intracranial haemorrhage is the most common cause of death.
Laboratory findings Partial thromboplastin time (PTT) is an
effective screening test for classical haemophilia. It gives abnormal results
when factor VIII is about 25% of the normal value. Platelet count and platelet
function tests such as bleeding time and thrombin time are normal.
Thromboplastin generation test (TGT) and prothrombin consumption test (PCT) are
too sensitive and give abnormal results even in very mild haemophilia.
Assay of factor VIII is the diagnostic test. Inhibitors of
factor VIII are detected in severely affected young patients. These are
specific IgG antibodies to factor VIII.
2. Haemophilia B
(Factor IX deficiency)
Haemophilia B is an inherited deficiency of factor IX and is
an X-chromosome linked disorder like haemophilia A. Haemophilia B is five times
less frequent than haemophilia A. Clinically, haemophilia B is
indistinguishable from the classical haemophilia but is generally a milder
form. The therapy for both the haemophilias being different, it is necessary to
differentiate between the two disorders.
Laboratory findings As in haemophilia A, a prolonged PTT,
normal thrombin time and normal bleeding time is observed in haemophilia B
patients. Prothrombin time is nor-mal in most cases. Factor VIII level is
normal whereas factor IX is deficient and is diagnostic.Antibodies to factor IX
may be seen only in patients undergoing long term therapy.
3. Haemophilia C
(Factor XI deficiency)
This is a rarely inherited bleeding disorder. The symptoms
are similar to those of the other haemophilias. The severity of the disease is
not related to the level of factor XI.
Laboratory findings These are similar to the other
haemophilias, and the diagnosis depends on the assay of factor XI.
4. von Willebrand
syndrome
von Willebrand syndrome (VWS) is one of the commonly
occurring inherited coagulation disorders. Like haemophilia A, VWS is also
related to the abnormality or the deficiency of factor VIII. Factor VIII is a
complex of two molecules: VIII:C and VIII:Ag.
(i) A small active molecule is the factor VIII
coagulant-antigen (VIII: Ag). Deficiency of this fraction leads to haemophilia
A
(ii) A larger fragment is called von Willebrand factor
(vWF), which is synthesized by endothelial cells and megakaryocytes. The vWF
circulating in the blood binds with factor VIII: Ag. It plays a carrier role
for the smaller active fraction and protects it from proteolytic destruction.
The main role of vWF is in the adhesion of platelets to foreign surfaces such
as glass, especially after vessel injury. .
Clinically, the patients with vWS characteristically bleed
from mucous membranes and cutaneous sites. Easy bruising and excessive bleeding
following dental extractions and tonsillectomy is common. Unlike classical
haemophilia, bleeding in the joints and deep muscles is not observed in vWS
except in severe cases. Gastrointestinal bleeding and menorrhagia are also
common.
Laboratory findings The diagnosis of vWS is difficult. The
routine laboratory screening tests are of limited value. Generally, bleeding
time and PTT are abnormal. The PCT (prothrombin consumption test) is usually
abnormal. Platelet adhesion and aggregation tests are more consistently
abnormal. Factor VIII:Ag is often reduced. For more specific diagnosis, rocket
immunoelectrophoresis is performed using an antibody to WF.
5. Other inherited
deficiencies
Inherited deficiencies of coagulation factors other than
those described above are very rare.
(a) Deficiency of
factor VII may be associated with the tendency of severe bleeding. A
prolonged prothrombin time with normal PTT and thrombin time is suggestive.
Specific factor VII assay should confirm the diagnosis.
(b) Deficiencies of
factor XII, HMWK or prekallikrein show very mild bleeding tendencies. The
laboratory tests show a prolonged activated PTT, normal prothrombin time and
normal thrombin time. If factors VIII and IX are suspected, then specific
assays of these factors should be performed.
(c) Deficiency of
factor X is not clinically distinguishable from that of factor VII. The
severity of the disease may vary. In most cases activated PTT and prothrombin
time are prolonged. Stypven time test should be performed to differentiate
between the two deficiencies. The test involves use of venom of the snake
Vipera russelli (Russell's viper). It acts directly on factor X to convert it
to factor Xa in the absence of other clotting factors. A prolonged Stypven time
in the presence of a prolonged prothrombin time is indicative of factor X
deficiency.
(d) Deficiency of
factor V is quite rare. The laboratory tests show prolonged prothrombin
time, PTT and TGT. Coagulation time may be abnormal.
(e) In factor XIII
deficiency, the laboratory results are almost normal. The diagnostic test
is based on solubility of the unstabilised fibrin clot in a five molar urea
solution or 1% mono-chloroacetic acid.
(f) Fibrinogen
deficiency is a rare inherited disorder but may lead to severe bleeding.
Laboratory results show abnormality in all the tests which have a fibrin clot
as the end point, e.g.. prothrombin time, thrombin time and PTT. The PCT and
TGT are normal except in severe cases.
(g) Prothrombin
deficiency is quite rare. The laboratory findings show prolonged
prothrombin time and PTT. Bleeding time, platelet count, clot retraction and
thrombin time are normal. Diagnosis is made by the specific assay for
prothrombin
II. Acquired
Disorders
1. Vitamin K
deficiency
Deficiency of vitamin K leads to defects in the synthesis of
coagulation factors VII, IX, X and prothrombin, all of which are dependent on
vitamin K for their synthesis. Vitamin K is normally obtained in two ways;
through the dietary intake of the vitamin produced by plants, and the vitamin
synthesised by the intestinal bacteria.
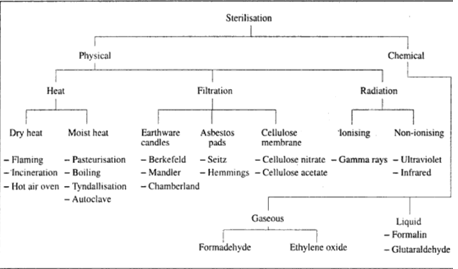
Vitamin K deficiency may result from
inadequate diet, intestinal malabsorption, biliary obstruction or gut
sterilisation. Haemorrhagic disease of the new-born may occur in neonates.
Vitamin K deficiency may be intentionally induced by the administration of
anticoagulant drugs such as coumarin. These drugs are administered orally and
are absorbed in the blood through the gastrointestinal tract. The level of the
anticoagulant in the blood is regulated in such a way that the prothrombin time
ratio is maintained at 1.5 (For example, prothrombin time of patient's plasma
is 15 seconds when that of the control is 10 seconds).
2. Heparin therapy
Heparin is a fast-acting mucopolysaccharide which interferes
with coagulation by inhibiting the action of factors lla, Xla, XIla and XIII by
blocking the conversion of fibrinogen to fibrin. It also inhibits platelet
aggregation. Heparin therapy is used in the treatment of thrombosis so that the
coagulation is extended with minimum of bleeding. The anticoagulant activity of
the heparin treated plasma is best monitored with the help of activated partial
thromboplastin time (APTT). The desired range of APTT is similar to that in the
oral anticoagulant therapy i.e. 1.5 times that of the control.
3. Diffuse
intravascular coagulation (DIC)
DIC syndrome may result from a wide variety of pathological
processes which lead to activation of the coagulation system.
Intravascular fibrin deposits may be produced with excessive
consumption of coagulation factors. Reduction in the level of coagulation
factors in turn leads to imbalance in the haemostatic mechanism and
uncontrolled bleeding may start. This process is often accompanied by
fibrinolysis which increases the bleeding tendency. The aetiological agents of
DIC include sepsis, neoplasms, autoimmune diseases, haematological diseases,
obstetric problems and intravascular haemolysis.
Laboratory findings
in DIC vary widely and depend on the cause and its severity. Generally,
prothrombin time, thrombin time and PTT are increased. Most cases of DIC are
associated with thrombocytopenia with leucocytosis. Schistocytes (fragmented
red cells) may be seen in the peripheral blood smear.
4. Lupus-type
anticoagulants
Some patients with systemic lupus erythematosus and other
wide variety of disorders and those undergoing therapy with drugs such as
phenothiazine, develop coagulation inhibitors known as lupustype
anticoagulants.
These substances inhibit the conversion of factor X to factor
Xa. The lupus-type anticoagulants produced under various conditions may not be
identical, but they are antibodies of either IgG or IgM type. The peculiar
feature of these anticoagulants is that they rarely show a clinical bleeding
tendency unless there is another pre-existing or additional haemostatic
abnormality. The laboratory result show abnormal prothrombin time, thrombin
time and PTT.
III. Inherited
Disorders of Platelet Function
1. Glanzmann's
thrombasthenia
In this disorder, the platelet count and individual platelet
morphology is normal, but they show a characteristic tendency to resist
clumping together. This results in inadequate platelet plug formation and is
due to an abnormality in the surface membrane glycoproteins. Clinically, the
bleeding can
be very severe. The laboratory tests show abnormal bleeding
time, prothrombin consumption test and clot retraction.
2. Bernard-Soulier
syndrome
This inherited disorder is due to the absence of some
membrane glycoproteins which are essential for platelet adhesion. The
laboratory findings include abnormally large (74 um) platelet forms, prolonged
bleeding time and reduced platelet adhesion to glass. The clot retraction is
normal.
3. Storage granule
abnormalities
Some platelet disorders involve a deficiency or abnormality
of one or more types of storage granules. In most cases, platelet release
function after stimulation and platelet aggregation are affected.
IV. Acquired
Disorders of Platelet Function
1. Drug Induced disorders A large number of drugs influence
platelet function. Aspirin and its derivatives are the principle causes of such
disorders. Other examples include antibiotics such as penicillins and
cephalosporins; analgesics and anti-inflammatory agents like ibuprofen; and
other miscellaneous drugs such as heparin. The platelet function usually
returns to normal when administration of causative agent is discontinued.
include acute and chronic leukaemias, haemorrhagic
thrombocythaemia, myelofibrosis, autoimmune diseases, systemic lupus
erythematosus and anaemia.
V. Quantitative
Platelet Disorders
1. Thrombocytopenia
A reduced number of circulating platelets (thrombocytopenia)
can result from:
(1) Decreased production of platelets Decreased production
of megakaryocytes or ineffective platelet production due to vitamin B12
deficiency can lead to thrombocytopenia.
(ii) Disorders of distribution This can occur due to
conditions such as hypothermia or transfusion of stored blood.
(iii) Platelet destruction A wide variety of conditions can
lead to platelet destruction. Infection, tissue injury, snake bite, thrombotic
thrombocytopenic purpura, autoimmune diseases, liver disease and malignancies
are some of the conditions that can cause platelet destruction.
2. Thrombocytosis
Increased platelet counts or thrombocytosis may result from a benign, reactive
process or may be associated with a myeloproliferative disorder. In most cases,
platelet stimulation and aggregation is affected.







If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..