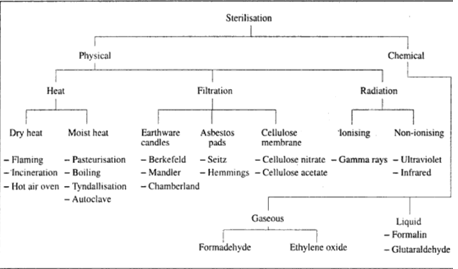
CHEMICAL STERILIZATION (DISINFECTANTS AND ANTISEPTICS)
Mode of Action of Chemical Agents
Chemical agents act on microorganisms in the following ways
MAJOR GROUPS OF DISINFECTANTS
Chemical agents act on microorganisms in the following ways
MAJOR GROUPS OF DISINFECTANTS
- Alcohols
- Aldehydes
(a) Formaldehyde
(b) Glutaraldehyde
(b) Glutaraldehyde
- Phenolic Compounds
- Chlorxylenols
- Salts of Heavy Metals
- Chlorhexidine (Hibitane)
- Halogens
(a) Hypochlorites
(b) Iodophores These consist of iodine
(c) Iodine As alcoholic tincture of iodine
Quaternary Ammonium Compounds
GASEOUS STERILIZATION
(b) Iodophores These consist of iodine
(c) Iodine As alcoholic tincture of iodine
Quaternary Ammonium Compounds
GASEOUS STERILIZATION
- Ethylene Oxide
- Formaldehyde
LABORATORY EVALUATION OF DISINFECTANTS
- the Kelsey Maurer's method.
CHEMICAL STERILIZATION (DISINFECTANTS AND ANTISEPTICS)
Various
disinfectants and antiseptics are used for chemical sterilization. They are
divided into a number of chemical groups for specific purposes. All chemical
agents of disinfection take time to act.
The rate of disinfection is approximately logarithmic, with a plot of the logarithm of the number of survivors against unit time giving straight line over most of the curve. This means that a constant proportion of surviving bacteria are killed per unit of time.
The rate of disinfection is approximately logarithmic, with a plot of the logarithm of the number of survivors against unit time giving straight line over most of the curve. This means that a constant proportion of surviving bacteria are killed per unit of time.
The actual
rate of kill varies due to certain factors, e.g., the nature of the
disinfectant and concentration used. Environmental conditions also affect the
efficiency of the chemical disinfectants, e.g., the presence of organic matter,
the pH of solution and the possible inactivation of chemical compounds such as
soap.
Mode of Action of Chemical Agents
Chemical agents act on microorganisms in the following ways:
1.
Interfering with the enzymatic system of the organism.
2.
Coagulation of proteins.
3.
Disruption of cell membrane.
4. Oxidative
damage.
MAJOR GROUPS OF DISINFECTANTS:Many different compounds are used as disinfectants, the major groups are:
Alcohols
Alcohols act
by denaturing proteins. Absolute alcohol is not a very effective disinfecting
agent due to its poor penetrating power. When diluted with water to a
concentration of 70 %, it has optimum activity as a skin antiseptic and it is
commonly used prior to injection or vain puncture. It is used as an antiseptic.
Aldehydes
(a) Formaldehyde
Formaldehyde is supplied as 40% solution and known as formalin. It is highly bactericidal and active against spores. It is used in liquid form or in gaseous form when humidity must be around 50%. Its extreme irritating and toxic property is the major disadvantage. It is useful for disinfecting rooms, safety cabinets (fumigation) and sometimes for aspirators and other anaesthetic equipment's.(b) Glutaraldehyde
This is used as a 2% buffered solution (Cidex)) and it is highly effective against all bacteria, tubercle bacilli and spores. It is much less irritant than formaldehyde but it is expensive. It has a low penetrating power but useful for items that cannot withstand heat such as endoscopes.Phenolic Compounds
Phenol or
carbolic acid is the oldest known disinfectant. Although, the original chemical
is no longer used, some of the compounds derived from it constitute the
phenolic substitutes. It is used usually at a concentration of 2-3%. Phenolics
are also effective against spores. Their unpleasant odour and tissue irritation
preclude their use on the skin. Phenolics such as 'Sudol', 'Hycolin', and 'Izal
are however, widely used as good antiseptics when diluted.
Chlorxylenols
The best
known of this group of disinfectants is dettol. They differ from other phenolic
compounds by being non-irritating, and can be applied to skin and tissues. They
are very active against Gram negative and Gram positive bacteria but not
against tubercule bacilli and spores. They are moderately inhibited by organic
matter.
Salts of Heavy Metals
Salts of
heavy metals, e.g., mercuric chloride, are required in high concentrations to
achieve any sig. nificant activity. They are slow acting and are mostly
bacteriostatic.
Chlorhexidine (Hibitane)
This is a
widely used skin disinfectant in alcoholic solution. It is very active against
a wide range of organisms, but aqueous solutions are much less effective due to
poor activity against spores, tubercule bacilli, and some Gram negative
bacteria such as Alcaligenes, Flavobacteria and some Pseudomonas. It is usually
used as hand cream in the laboratory after washing hands with soap and water.
Halogens
(a) Hypochlorites
These include such popular antiseptics as milton, chloros and domestos. They are derivatives of chlorine which is liberated from the solution during their action. As disinfectants, hypochlorites are bactericidal against vegetative bacteria, spores and viruses, but less active against tubercule bacilli. They are relatively inactivated by organic matter.(b) Iodophores These consist of iodine
detergent complexes and include such well known brands as Wescodine, Betadine and Pevidine. They are much less irritant to the skin than free iodine and do not stain. They are used for cleaning wounds and as a general purpose laboratory disinfectant for discard jars(c) Iodine As alcoholic tincture of iodine
it is highly active against Gram positive organisms and so is used as a skin antiseptic. It stains the skin.Quaternary Ammonium Compounds
These include agents such as cetrimide, bromide and benzalkonium chloride. They have antibacterial and detergent properties and are active against Gram positive bacteria and slightly active against tubercule bacilli and spores.This antibacterial activity is antagonised by soaps and certain organisms, e.g., Pseudomonas. They are very useful in catering industry for washing cutlery, and in hospitals for cleaning wounds. Savlon, a popular antiseptic, is a mixture of cetrimide and chlorhexidine and is active against Gram negative bacteria.
GASEOUS STERILIZATION:
Gaseous disinfectants (alkylating agents) are used for the sterilisation or disinfection of items of hospital equipment that is bulky or heat-labile. The most widely used gases are ethylene oxide and formaldehyde.Ethylene Oxide
Ethylene oxide has a boiling point of 10.8°C, so it is a gas at room temperature. It is highly inflammable and explosive in pure form, but is safe to handle when mixed with carbon dioxide. It is effective in the killing of all bacteria, including tubercle bacilli and spores.
To be
effective, however, the humidity and temperature must be carefully controlled
within narrow limits. It is highly toxic on contact with the skin or mucous
membrane.
Materials that have been sterilized with ethylene oxide must be set
aside in detoxification chambers for a few days to allow the gases to
dissipate. It is frequently used to sterilize heart lung machines and plastic
items, e.g., catheters.
Formaldehyde
It is highly bactericidal. As gas, it is used as 40 % formalin with humidity at around 50%. It is highly irritant. it is used occasionally to fumigate rooms and disinfect respirators.LABORATORY EVALUATION OF DISINFECTANTS
The aim of
evaluation of a disinfectant is to define the capabilities of the disinfectant
and to determine reasonable and practicable concentrations for routine use.
There are many factors that influence bactericidal activity, and so, conditions
of testing must simulate practical usage conditions.
A suspension test, the 'Rideal Walker or the
'Phenol Coefficient test,' is an old method but hardly related to conditions
obtainable in the laboratories. For this reason, it is not very satisfactory
.
Other tests
such as, 'In-Use Test' and 'Capacity Test' are quite satisfactory. All quantitative tests for bactericidal activity involve the serious technical difficulty of enumerating the few surviving organisms as disinfection proceeds.The In-Use Test, which is simple and easy to perform, is outlined below: In-Use test method This is the Kelsey Maurer's method.
Stage 1 l ml disinfectant solution in use is taken from the jar with a sterile
pipette.
Stage 2 The
1 ml sample is added to 9 ml diluent in a sterile universal container. The
diluent should be selected according to the group to which the disinfectant
belongs. This in effect means that the action of the disinfectant should be
stopped using the appropriate inactivator. For general purposes, use 0.5% Tween
80
Stage 3 The
bottle of diluted disinfectant is transported to the laboratory within an hour
of the addition of the disinfectant. A separate sterile Pasteur pipette is used
to withdraw a small quantity of the disinfectant/diluent/mixture and to place
10 drops, separately, on the surface of each of two well-dried nutrient agar
plates. A 50 dropper pipette may be used in place of graduated pipette.
Stage 4 The two plates are incubated:
(a) One
plate is incubated for three days at 32 or 37°C, whichever is more convenient.
(The optimum temperature for most pathogenic bacteria is 37°C but those which
have been damaged by disinfectants often recover more readily at 32°C.)
(b) The
second plate is incubated for seven days at room temperature. Stage 5 After
incubation the plates are examined and bacterial growth is recorded. In-Use
test result The presence of bacterial colonies on one or both of a pair of
plates is evidence of the survival of bacteria in the particular jar, from
which the sample was taken. One or two colonies on the plate may be ignored. A
disinfectant is not a sterilant. The presence of a few live bacteria is to be
expected. The growth of five or more colonies should arouse suspicion and may
be indicative of poor bactericidal activity.





If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..