Anemia
Anemia is not a specific disease. It is a condition in which oxygen carrying capacity of blood is reduced. Anemia is
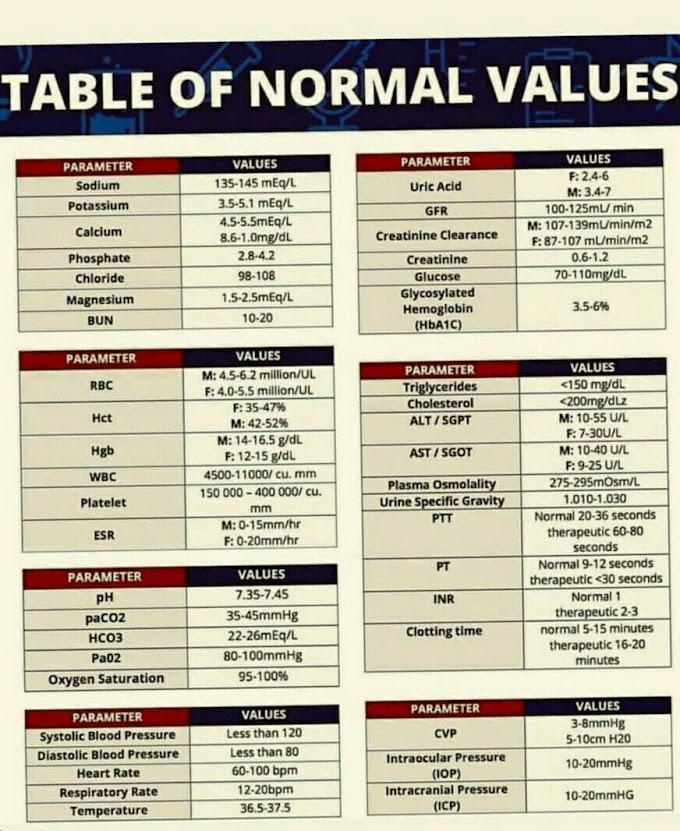
always a sign of an underlying disease, and never a diagnosis. A red cell count
of less than 4.0 million/cu.mm (ul) in males and 3.5 million/cu.mm (ul) in
females, or hemoglobin content of less than 10.8 g per 100 ml (108g/ L) in
males and 9.5 g/100 ml (95 g/L) in females is an indication of anemia.
Patients with anemia have similar
clinical symptoms
irrespective
of the cause. Fatigue, breathlessness, dizziness and headache are some of the
common complaints.
Anemia may be caused due to the following
factors
- Increased haemolysis.
- Diminished erythropoiesis.
- Blood loss
Increased haemolysis may be due to hereditary defects
such as spherocytosis, or sickle cells, which reduce the life span of the red
cell; or may be acquired by the action of haemolytic agents.
Diminished erythropoiesis is either due to a nutritional
deficiency or due to the marrow failure. The nutritional factors essential for
erythropoiesis are iron, cobalt, copper, vitamin B12, folic acid, pyridoxine,
riboflavin, nicotinic acid, Vit C, proteins and some hormones. The deficiency
of these factors may be dietetic, due to defective absorption or due to
increased demands, (e.g., during pregnancy or period of growth).
Failure of
marrow may be endogenous or due to extraneous toxic factors such as chemicals
and drugs. Blood loss may be brought about by trauma or disease and may be
acute or chronic in nature.
CLASSIFICATION OF ANEMIA
Generally, anemia are classified on the basis of the appearance of the red cells
(morphological classification) or depending on the physiological cause
(aetiological classification).
MORPHOLOGICAL CLASSIFICATION OF ANEMIA
Morphological
classification of anemia depends on the examination of blood which includes
the determination of hemoglobin, enumeration of red cells, red cell indices
and the examination of the peripheral blood smear.
The levels of hemoglobin and red cell count determine the severity of anemia while the examination of smear will give information about the size of the red cells, their hemoglobin content and presence of abnormal red cells. The red cell indices provide important guidelines for morphological classification of anemia.
The levels of hemoglobin and red cell count determine the severity of anemia while the examination of smear will give information about the size of the red cells, their hemoglobin content and presence of abnormal red cells. The red cell indices provide important guidelines for morphological classification of anemia.
1.Macrocytic, normochromic anemia:- MCV 100 to 160 cu.microns (FL) MCHC 32 to 36 %
Causes
(a)
Deficiency of Vitamin B 2 or folic acid,hepatic disease, or antimetabolite
drugs. The bone marrow shows abnormal red cell maturation, megaloblastic
(increased red cell size) changes.
(b) Chronic
liver disease, hypothyroidism etc. where bone marrow does not show abnormal
megaloblastic changes.
2. Normocytic, Normochromic Anemia:- MCV 80 to 100 cu.um (fL), MCHC 32 to 36 %
Causes
(a) Sudden
blood loss
(b)
Haemolytic anaemias
(c)
Haemoglobinopathies
(d) Aplastic anaemia
3. Microcytic Normochromic Anemia:- MCV 69 to 80 cu.um (fL), MCHC 32 to 36 %
Causes
(a)
Inflammatory conditions.
(b) Toxic
drugs and chemicals
(c)
Malignancy
(d)
Endocrine disorders
4. Microcytic Hypochromic Anemia:- MCV 60 to 80 cu. um (FL), MCHC 20 to 30 %
Causes
(a) Iron
deficiency due to blood loss, improper gastrointestinal absorption, excess
demand.
(b)
Miscellaneous, such as lead poisoning,thalassaemia.
5. Macrocytic Hypochromic Anemia:- MCV
more than 100 cu. um (fL), MCHC less than 30 % Causes Deficiency of iron
associated with deficiency of Vitamin B12 or folic acid.
ETIOLOGICAL CLASSIFICATION OF ANEMIA
1.Anemia Resulting from Excessive Destruction of Red Cells:- Due to intracellular defects Hereditary defects of red cell membrane (e.g. spherocytosis,
2.Autoimmune haemolytic anemia (AIHA) :-In AIHA, the defect is extracorpuscular. These anemia occur because of
the production of antibodies against the patient's own red cells. The
classification of their causes is shown in Table 5.3. The warm antibodies react
better at 37°C while cold antibodies are active at 4°C. Warm AIHA Clinical
features It is a haemolytic anemia of varying severity occurring at any age.
The spleen is enlarged. Warm AIHA is frequently associated with other
autoimmune disorders such as systemic lupus erythematosus (SLE).
Laboratory findings
1.
Peripheral blood smear is typical of haemolytic anaemia and shows prominent spherocytosis.
2. Direct
Coomb's test is positive.
3.
Antibodies are best detected at 37°C.
Cold AIHA
Clinical features:-The patients have chronic haemolytic anaemia which
increases in cold weather. Peripheral circulation (tip of the nose, ears,
fingers, toes) may be affected due to agglutination of red cells in small
vessels. Infections such as infectious mononucleosis or mycoplasma pneumonia
may precipitate cold AIHA.
Iso-immune haemolytic anemia:- In this type of anaemia, antibodies
produced by one person react with the red cells of another.
This can
occur in: Transfusion of ABO incompatible blood
(ii) Haemolytic disease of the new-born(HDN)
1.Drug-induced immune haemolytic anaemia:- Many drugs can induce the formation
of antibodies either against the drug itself or against red cell antigens.
These antibodies, in the presence of complement, can bring about lysis of red
cells. Drugs which are known to cause haemolytic anaemia include penicillin,
cephalothin, phenacetin and methyl DOPA. Haemolytic anaemia gradually
disappears when the drug is discontinued.
Paroxysmal nocturnal haemoglobinuria (PNH):-This occurs due to an acquired defect
of the red cell membrane that makes it susceptible to complement mediated lysis
of red cells. The defect is rare, haemolysis is intravascular and usually
occurs at night (nocturnal). PNH is diagnosed by Ham's serum acid test
(demonstration of red cell lysis at low pH). White cell, platelet and
reticulocyte counts are low.
Paroxysmal cold haemoglobinuria (PCH):- This is similar to PNH but
haemolysis occurs after exposure to cold. The patient's blood contains an
antibody called Donath-Landsteiner antibody which binds red cells in the cold.
The lysis with complement occurs at 37°C. Syphilis and viral infections are
predisposing factors.
Classification
of auto-immune hemolytic anaemias (AIHA)
|
|
Warm antibody
|
Cold antibody
|
A.
Idiopathic
B.
Secondary to
1.systemic
lupus-erthematous (SLE)
2.
other auto_immune disease
3.chronic
lymphatic leukemia(CLL)
4.lymphoma
5.drug
such as methyl DOPA
|
A. Idiopathic
. Secondary to
1.infection mononucleosis
2. mycoplasma pneumonia infection
3. lymphoma
4 .parxymal cold haemoglobinuria (RARE)
|
3.Miscellaneous haemolytic anemia:- Various causes other than those
mentioned earlier can give rise to haemolysis and haemolytic anemia.
These include:
(I) Malaria.
(ii)
Bacterial infections
(iii)
Extensive burns.
(iv)
Overdose with oxidizing drugs
(v) Chemical
poisoning
(vi) Snake and
spider bites.
4. Aplastic Anemia:-Aplastic anaemia results from aplasia of bone marrow.
Haemopoiesis is affected causing reduction in the counts of all blood cell
series (anaemia, leucopenia, thrombocytopenia, collectively called
pancytopenia).
The
causes of aplastic anaemia are divided into two groups:
|
|
(i) Primary causes
|
(ii) Secondary causes
|
(a) Congenital.
(b) Idiopathic-without any obvious
precipitating cause.
|
(a) Exposure to radiation such as
radiotherapy, radioactive isotopes.
(b) Chemicals: Organic solvents like
benzene, hair dyes.
(c) Drugs: Such as cyclophosphamide,
|
6 mercaptopurine,
chloramphenicol.
(d)
Infections: Viral hepatitis caused by hepatitis A virus and other related
viruses.
Clinical features:- It can occur at any age, but is more common around 30 years of age. Infections, either localised (e.g. of the mouth and throat) or generalised, are very common. The lymph nodes, liver and spleen are not enlarged.
Laboratory findings :-
1.
Peripheral blood smear shows normocytic or macrocytic (MCV increased) and
normochromic red cells. The reticulocyte count is low.
2.
Leucopenia: There is a marked decrease in granulocytes, though their morphology
is normal.
3. Platelet
count is very low (thrombocytopenia).
4. Peripheral
blood smear shows no abnormal cells.
5. Bone
marrow shows hypoplasia. There is a fatty degeneration of the haemopoietic
tissue. The main cell types seen are lymphocytes and plasma cells.
5. Anemia in Systemic
Disease:- Anemia
may appear as one of the symptoms in various systemic diseases of organs other
than bone marrow.
These include:-
(i)Malignant
disease.
(ii)
Rheumatoid arthritis, SLE and other connective tissue disorders.
(iii)
Chronic renal failure.
(iv) Liver
disease. (v)Alcoholism.
(vi)
Hypothyroidism.
(vii)
Tuberculosis.





If you have any queries related medical laboratory science & you are looking for any topic which you have have not found here.. you can comment below... and feedback us if you like over work & Theory
.
Thanks for coming here..